CDRH COVID-19 Diagnostic Templates (Molecular and Antigen) - Antigen Diagnostic Template
0910-0595_CDRH_antigen_template.docx
Authorization of Medical Products for Use Emergencies
CDRH COVID-19 Diagnostic Templates (Molecular and Antigen) - Antigen Diagnostic Template
OMB: 0910-0595
OMB: 0910-0595
Exp. date 9/30/2025
Contains Nonbinding Recommendations
Template for Developers1 of Antigen Tests
This template provides the Food and Drug Administration’s (FDA) current recommendations concerning what data and information should be submitted to FDA in support of a pre-Emergency Use Authorization (EUA)/EUA request for a SARS-CoV-2 antigen test. FDA generally recommends that the following validation studies be conducted for a SARS-CoV-2 antigen test: limit of detection (LoD)/analytical sensitivity, cross-reactivity/analytical specificity, microbial interference, and a clinical agreement study.
As described in the FDA guidance document: Policy for Coronavirus Disease-2019 Tests During the Public Health Emergency (Revised),2 FDA is providing recommendations in this and other EUA templates regarding testing that should be performed to ensure appropriate analytical and clinical validity, including descriptions of appropriate comparators, for different types of tests. The EUA templates3 are intended to help test developers provide recommended validation data and other information to FDA, but alternative approaches can be used.
This template reflects FDA’s current thinking on the topic, and should be viewed only as recommendations, unless specific regulatory or statutory requirements are cited. The use of the word should, means that something is suggested or recommended, but not required. For more information about EUAs in general, please see the FDA guidance document: Emergency Use Authorization of Medical Products and Related Authorities.4
Test developers interested in pursuing an EUA may submit a pre-EUA to begin discussions with the FDA or may submit an EUA request to CDRH-EUA-Templates@fda.hhs.gov.
GENERAL INFORMATION ABOUT THIS TEMPLATE
Text highlighted in yellow [Text] should be completed by the test developers as applicable to their specific test. Text in bold outlines the FDA’s additional recommendations for the developers’ consideration when completing the suggested information in each section.
Not all portions of this template may be relevant for all developers/tests. FDA recommends developers complete all portions that are relevant to facilitate a streamlined review.
This template addresses tests intended for use with respiratory samples and saliva; if you are considering other sample types, please contact FDA at CDRH-EUA-Templates (covid19dx@fda.hhs.gov) to discuss your validation strategy.
A test authorized under an EUA is only authorized for emergency use while the EUA is in effect.
We plan to update the template as appropriate as we learn more about COVID-19 and gain experience with the EUA process for these kinds of tests.
A developer that has provided data to the FDA, may grant a right of reference to other developers, either broadly or to individual developers, to leverage that data. A right of reference provides a developer the ability to rely upon, and otherwise use, existing information in one regulatory submission for the purpose of supporting a different regulatory submission. In these cases, if the data is applicable to the new developer's test, the new developer may not have to repeat that validation for its submission to the FDA or FDA may recommend a bridging study. Any developer seeking to leverage data regarding another developer’s EUA-authorized assay must obtain a right of reference from that developer.
EXAMPLE TEMPLATE:
PURPOSE FOR SUBMISSION
Emergency Use Authorization (EUA) request for distribution and/or use of the [test name] to for the in vitro qualitative detection of antigen from SARS-CoV-2 in [add all sample types, e.g., nasopharyngeal swabs, oropharyngeal swabs, sputa, BAL, etc. and specific brands of viral transport media (VTM), as applicable] [select appropriate testing population, e.g., from patients who are suspected of COVID-19 by a healthcare provider within the first (insert number) days of symptom onset, or for screening of individuals without symptoms or other reasons to suspect COVID-19 infection, if applicable]. Test results are required to be reported in accordance with local, state, and federal regulations.
MEASURAND
Specific antigen(s) from the SARS-CoV-2 [please specify the targeted antigen(s)].
APPLICANT
[Official name, address, and contact information (including phone number and email address) of applicant and primary correspondent.]
PROPRIETARY AND ESTABLISHED NAMES
Proprietary Name - [test name]
Established Name - [test name]
REGULATORY INFORMATION
Approval/Clearance Status:
The [test name] test is not cleared, CLIA waived, approved, or subject to an approved investigational device exemption.
[If the test has been previously reviewed in an EUA request or pre-EUA submission, please provide the submission number.]
Panel Code: MI for Microbiology tests
Review Group: Division of Microbiology Devices/VIR1
Product Code:
QKP - coronavirus antigen detection test system
PROPOSED INTENDED USE
Intended Use (IU):
The proposed IU will be finalized based on, among other things, the data provided and recommendations from Public Health authorities at the time of authorization. Example text is provided below for a qualitative antigen test but may be adapted according to the specific emergency situation addressed by the device, proposed intended use population, testing sites, or performance characteristics.
The [test name] is a [specify test technology, such as lateral flow immunoassay] intended for the qualitative detection of [protein name] antigen from SARS-CoV-2 in [describe all the sample types] [with specific brand of transport media, as applicable] [select appropriate testing population, e.g., from patients who are suspected of COVID-19 by a healthcare provider within the first (insert number) days of symptom onset or for screening of individuals without symptoms or other reasons to suspect COVID-19 infection, if applicable]. Testing is limited to laboratories certified under the Clinical Laboratory Improvement Amendments of 1988 (CLIA), 42 U.S.C. § 263a, that meet the requirements to perform [insert testing complexity, e.g., moderate complexity, high complexity, or waived tests. This test is authorized for use at the Point of Care (POC), i.e., in patient care settings operating under a CLIA Certificate of Waiver, Certificate of Compliance, or Certificate of Accreditation.].
Results are for the identification of SARS-CoV-2 [protein name] antigen. Antigen is generally detectable in [sample type] during the acute phase of infection. Positive results indicate the presence of viral antigens, but clinical correlation with patient history and other diagnostic information is necessary to determine patient infection status. Positive results do not rule out bacterial infection or co-infection with other viruses. The agent detected may not be the definite cause of disease.
Laboratories within the United States and its territories are required to report all results to the appropriate public health authorities.
Negative results should be treated as presumptive, and do not rule out SARS-CoV-2 infection and should not be used as the sole basis for treatment or patient management decisions, including infection control decisions. Negative results should be considered in the context of a patient’s recent exposures, history, and the presence of clinical signs and symptoms consistent with COVID-19, and confirmed with a molecular assay, if necessary, for patient management.
The [test name] is intended for use by [include intended user, e.g., qualified, and trained clinical laboratory personnel specifically instructed and trained in vitro diagnostic procedures].
The [test name] is only for use under the Food and Drug Administration’s Emergency Use Authorization.
Special Conditions for Use Statements:
For prescription use only
For in vitro diagnostic use
For Emergency Use Authorization only
Special Instruments:
The [test name] test is to be used with the [list all instruments, software, cameras, smart phone operating systems, other applicable instrumentation, etc.].
If your test system includes an instrument, the instrumentation manual should be submitted as part of the EUA request. If your test system includes an instrument that was not previously cleared, approved, or authorized by FDA, please see additional discussion in the Product Manufacturing section and note that additional labeling information may be discussed during the EUA review.
DEVICE DESCRIPTION AND TEST PRINCIPLE
Please provide a device description. Example text has been added under each of the sub-headings. Please modify the example text as appropriate for tests that use a different test principle. For new technologies, FDA may request additional detailed information so we can adequately assess the known and potential risks and benefits associated with the device.
Product Overview/Test Principle:
[Describe the technology of the test and how this technology works to identify the measurand (i.e., the test principle), the instruments/reader employed/required to perform the test from sample collection to result, and the sample types for which you claim to have specific performance characteristics, as described below. Please indicate if the test uses biotin-Streptavidin/avidin chemistry in any of the steps for coupling reagents. Please specifically state if your device is intended to be used with viral transport media and if so, provide the specific brands of transport media with which you have validated your device.]
The [test name] is a [description of technology (e.g., lateral flow, etc.)] test. The [test name] is designed to detect antigen from the SARS-CoV-2 in [list all the sample types] from [select appropriate testing population, e.g., from patients who are suspected of COVID-19 by a healthcare provider within the first (insert number) days of symptom onset or for screening of individuals without symptoms or other reasons to suspect COVID-19 infection, if applicable. The [test name] is validated for testing direct samples without transport media and/or testing samples in [specific brand or type, as applicable] transport media.
Description of Test Steps:
[List and describe in detail all of the steps of the test sequentially, from sample collection to assay report.]
[Step one]
[Step two]
[Etc.…]
Control Material(s):
[List all control materials (provided with the test kit and/or required but not provided with the test kit, e.g., sold as a separate kit) and describe what they are, how they are expected to work, where in the testing process they are used, and the frequency of use. If a control is commercially available, provide supplier’s name and catalog number or other identifier; if your device relies on external controls that are manufactured by a third party, please note that these controls should also be validated within your analytical and clinical studies, described below in Section J.]
Controls that will be provided with the test kit include:
An external positive control is needed to [describe need] and is used [describe use – please specify the concentration of the positive control relative to the LoD of your test (note that ideally the positive control concentration should be such that it is close to the LoD of your test) and specify frequency of use].
An external negative control is needed to [describe need] and is used [describe use – please specify the composition of the negative control and specify frequency of use].
A [other (e.g., sample adequacy, internal, etc.)] control is needed to [describe need] and is used [describe use – please specify the composition of the control and specify frequency of use].
Controls that are required but not provided with the test kit include [describe control – provide recommended sources of the control materials – either a separate control kit for purchase that you, the applicant, develops, or a control material that can be purchased from a third party]. This/these control(s) is/are needed to [describe need] and is/are used [describe use – please also specify frequency of use].
Please note that any control used with your device (provided with the kit or not) should be validated in the context of your analytical and clinical studies (i.e., your studies should include use of these controls). In instances where control material is not readily available through 3rd party vendors, FDA recommends that you include suitable control material with your device. External control materials are considered particularly important when good manufacturing practice (GMP) requirements are waived, and reagent stability studies are limited.
Test Result Reporting:
All test results are to be reported to healthcare providers and relevant public health authorities in accordance with local, state, and federal requirements, using appropriate LOINC and SNOMED codes, as defined by the Laboratory In Vitro Diagnostics (LIVD) Test Code Mapping for SARS-CoV-2 Tests5 provided by the Centers for Disease Control and Prevention (CDC). Core diagnostic data elements6 are to be collected for all tests, which have been defined by the Department of Health and Human Services (HHS), along with technical specifications for implementation for lab-based7 and non-lab-based8 tests.
INTERPRETATION OF RESULTS
All test controls should be examined prior to interpretation of patient results. If the controls are not valid, the patient results cannot be interpreted. [Appropriate control interpretation criteria should appear in your product labeling. If the test result involves the use of an algorithm/calculation when determining the final patient test result, please include a detailed description and any additional calibration materials that may be required.]
[Test name] Controls – Positive, Negative, and Others:
[Describe in detail the expected results generated, including the acceptance criteria, for all the controls described in Section G above. Describe the measured values (if applicable) for valid and invalid controls and outline the recommended actions the laboratory should take in the event of an invalid control result.]
Examination and Interpretation of Patient Sample Results:
[Describe when clinical sample test results should be assessed and outline the criteria for test validity.]
Example text: Assessment of [test name] results should be performed after the positive and negative controls have been examined and determined to be valid and acceptable. If the controls are not valid, the patient results cannot be interpreted.
[Clearly indicate how to interpret numeric test values (if applicable) as positive or negative for presence of COVID-19 antigen. If applicable, indicate how to identify indeterminate/inconclusive/equivocal results. When applicable, we recommend providing a table clearly describing the possible combinations of test result values for each detected antigen, if applicable, and controls. Describe how they should be combined into a final interpretation of the result for your test. If the test produces an equivocal or indeterminate result, please indicate what follow-up testing/process should be conducted, if applicable.]
[If you propose to report a quantitative value to healthcare providers, there may be additional considerations for the analytical and clinical validation of your device. Please contact FDA to discuss any validation proposals for a quantitative or semi-quantitative assay.]
PRODUCT MANUFACTURING
The [test name] has been validated using only the components referenced in this request and will not be changed after authorization without prior concurrence from the FDA.
Overview of Manufacturing and Distribution:
The product will be manufactured at [test developer’s name and FDA registration number (if applicable)] by [test developer’s name] personnel consistent with practices for the production of [types of devices] based on [type of quality system (e.g., 21 CFR 820 or ISO13485)]. Material manufactured by [test developer’s name] may be bottled and kitted by [packager name] manufacturing facility.
The current manufacturing capabilities include the ability to manufacture approximately [please insert the approximate number of tests/kits that can currently be manufactured per week at the manufacturing facility] products per week for distribution in the United States, however, in the event of a surge in demand this could be increased to [please insert the approximate maximum number of tests/kits that could potentially be manufactured per week at the manufacturing facility if there was a surge in demand] products per week within a [please specify in weeks/months the expected timeframe to increase product production, if conditions warrant] timeframe.
Under an EUA, certain sections of the 21 CFR Part 820 Quality System Regulation (QSR) requirements may be waived for an authorized product during the duration of the EUA, but FDA recommends that test developers follow comparable practices as much as possible, even if such requirements are waived. Please see recent letters of authorization for examples of which QSR requirements have been required.
[Please specify any instruments or other components of your test which are labeled as research use only (RUO) or are otherwise not labeled with the statement “For In Vitro Diagnostic Use” or a symbol found in a standard to the same effect.]
For distributed tests (i.e., tests intended to be performed in more than one laboratory location) that use an RUO instrument, please provide the following information, as applicable:
FOR AN RUO INSTRUMENT WHERE THE EUA REQUESTER IS NOT THE MANUFACTURER OF THE INSTRUMENT:
Please include in the instructions for use found in your test’s labeling, appropriate procedures, including acceptance criteria, that laboratory customers should follow to qualify the performance of the RUO instrument prior to use with your test.
These procedures could include wet testing of quantitated test material with your test, or confirmation that key specifications of the instruments that are applicable to your test are within an acceptable range. The quantitated virus material could either be positive control material included with your kit or commercially available positive virus control material. If commercially available material is not labeled with the statement “For In Vitro Diagnostic Use” or a symbol found in a standard to the same effect, then you should qualify lots of this material in-house and have a mechanism to notify laboratory customers which lots are appropriate to use for qualification (i.e., posting on a website). For the qualification protocol, you should include a recommendation to test multiple dilutions of virus material with your test, with, at minimum, 3 replicates per dilution. There should be at least one dilution near the LoD (i.e., within 3x LoD (3 times LoD)) of your test. The protocol should outline the acceptance criteria for each dilution tested.
[Please also provide the following labeling documentation with your request:
A "For Emergency Use Authorization only" label that users can affix to the instrument after it has been qualified. This can be provided as an Appendix in the assay instructions for use.
Please ensure that your test’s labeling either reproduces the parts of the instrument operating manual that are relevant to run your test or references the relevant sections of the manual.]
FOR AN RUO INSTRUMENT WHERE THE EUA REQUESTER IS THE MANUFACTURER OF THE INSTRUMENT:
[Please either provide the qualification protocol as described above or the following information to demonstrate your instrument meets the minimum quality system requirements for authorization:
The ISO 13485 certificate for the site where your instrument is manufactured.
A document mapping out the parts of your quality system that fulfill each of the following:
Subpart H (Acceptance Activities, 21 CFR 820.80 and 21 CFR 820.86),
Subpart I (Nonconforming Product, 21 CFR 820.90), and
Subpart O (Statistical Techniques, 21CFR 820.250).
Please provide the following labeling documentation with your request:
A “For Emergency Use Authorization only” label that the users can affix to the instrument after it has been qualified. This can be provided as an Appendix in the assay instructions for use.
The instrument operating manual. Please note that the manual should not include any unapproved, uncleared, or unauthorized uses.
An instrument manual addendum that can be distributed along with your EUA test kit. The addendum may have the following format:]
Instrument Operation Manual Addendum
For emergency use authorization only with the [test name].
The [test name] is authorized for use under the US Food and Drug Administration (FDA) Emergency Use Authorization (EUA) with the [name of instruments] for the [presumptive] qualitative detection of antigen protein from SARS-CoV-2 [intended use of test]. Refer to the [test name] instructions for use for additional information [provide hyperlink].
This instrument operation manual addendum applies to the instruments listed in Table 1 that are authorized for use with the [test name].
Table 1: Instruments Authorized for Emergency Use with the [test name]
-
Catalog Number
Product Name
Warnings:
This product has not been FDA cleared or approved; the product has been authorized by FDA as part of [test name] under an EUA for emergency use only by authorized laboratories certified under the Clinical Laboratory Improvement Amendments of 1988 (CLIA), 42 U.S.C § 263a.
[Test name] has been authorized only for the detection of antigen protein from SARS-CoV-2, not for any other viruses or pathogens.
The emergency use of [test name] is only authorized for the duration of the declaration that circumstances exist justifying the authorization of emergency use of in vitro diagnostics for detection and/or diagnosis of COVID-19 under Section 564(b)(1) of the Federal Food, Drug, and Cosmetic Act, 21 U.S.C. § 360bbb-3(b)(1), unless the declaration is terminated, or authorization is revoked sooner.
Components & Other Materials/Information Included with the Test:
Components manufactured by [test developer’s name and FDA registration number (if applicable)] and supplied with the test include:
[List all components and other materials/information included with your test, including a description of the reagents, volumes, concentrations, quantities, buffer components, etc.]
Example: Kit Components & Other Materials/Information Table
Kit Components & Other Materials/Information |
Main Reagents composition/ Matrix |
Concentration/ Quantity/Volume |
Manufacturer |
Test Cassette with test strip |
|
|
|
Negative control |
|
|
|
Positive control |
|
|
|
Calibrators |
|
|
|
Sample buffer (bottle) |
|
|
|
Transfer pipette |
|
|
|
Instructions for Use leaflet |
|
|
|
Packing materials |
|
|
|
Others, as applicable |
|
|
|
Components and Other Materials/Information Required but Not Included with the Test:
[List all components and other materials/information (e.g., instruments, reagents) not included with the test that must be supplied by the user to perform the test, with specific supplier names and catalog numbers or other identifiers for obtaining the components. Please include here all specific consumables that were validated for use with your device, that are not interchangeable with other products, and that are needed to guarantee device performance as established in the EUA validation studies listed in Section J below.]
Software Validation:
If you are introducing a system onto the market that has not been previously reviewed by FDA, we recommend providing evidence that the software has been validated to ensure that:
The inputs and outputs of the software are appropriate to fulfill the system and assay requirements;
All expected inputs produce the expected outputs for all functions critical for system operation; and
The system will be provided to the customer free of defects, or defects will be known and mitigated.
If this evidence is not available prior to authorization and the software and hardware have been designed and developed in a manner consistent with current GMPs (for additional information, please see the discussion of “Quality System Regulation/Medical Device Good Manufacturing Practices,” on the FDA website9), additional software validation documentation may be incorporated into the conditions of authorization. If changes which impact assay performance or safety and effectiveness of the system are needed to address validation failures post-authorization, an EUA supplement may be required under the conditions of authorization.
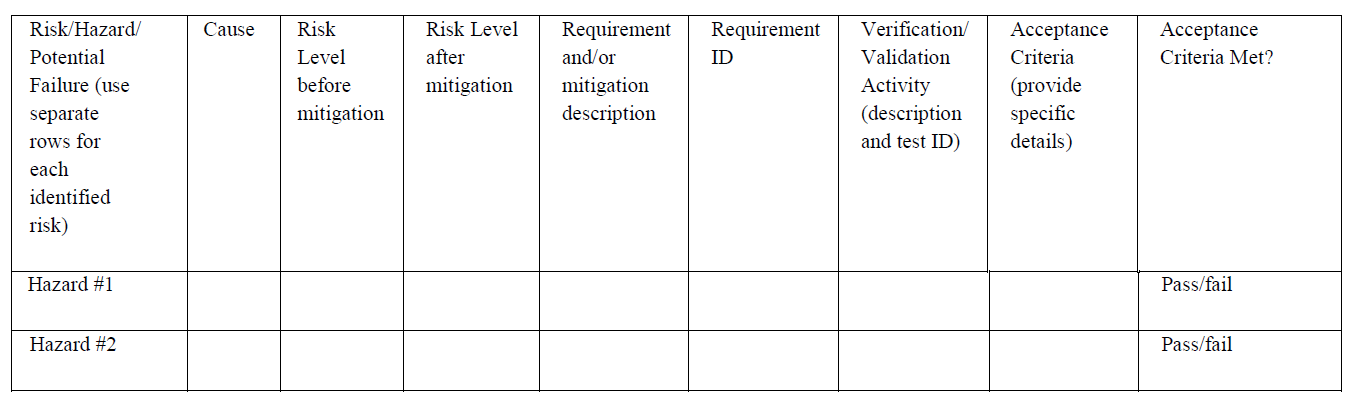
Below are examples of tables for providing system specific information and your evidence that specifications have been met (e.g., hazard analysis). Text in the tables is provided as an example only. [Please provide thorough functional descriptions of system software and instrumentation specifications needed to support the intended use of the test and provide evidence that specifications have been fulfilled.]
Example: System Specifications and Validation
Critical specifications: Description of the specification |
Evidence that the design of the system can fulfill the specification. This column should consist of system-level validation data. |
Optical system of each instrument sent to a user has sufficient dynamic range to appropriately differentiate between positive and negative test results |
|
Software displays appropriate result during test run |
|
If reader stores test result, software accurately stores and retrieves test results |
|
System has a defined lifetime where the user can expect the system to maintain performance as stated in the label |
|
Etc. |
|
Example:
Hazard Analysis
ID |
Hazard |
Adverse Effect |
Severity |
Potential causes of hazard |
Risk mitigation measure |
Risk of experiencing the hazard after mitigation |
1 |
Invalid result |
Delay in returning test result |
Low |
User inserts cartridge incorrectly |
Labeling noting correct orientation |
Low |
2 |
False result |
Wrong result returned to user |
High |
Incorrect alignment of test strip and optics; test strip inserted in the wrong orientation |
Mechanical design of reader input slot |
Moderate |
3 |
False negative result |
Wrong result returned to user |
High |
User reads test strip too early; incubation time not sufficient |
Labeling noting correct incubation time |
Moderate |
4 |
False result |
Wrong result returned to user |
High |
Incorrect alignment of test strip and optics; control line misinterpreted |
Software interprets data from optical system identifying a valid/invalid control |
Moderate |
5 |
False result |
Wrong result returned to user |
High |
Control reaction intensity is misinterpreted |
Software interprets data from optical system identifying a valid/invalid control |
Moderate |
6 |
False result |
Wrong result returned to user |
High |
Analyte reaction intensity is misinterpreted |
Software interprets data from optical system identifying a valid/invalid control |
Moderate |
If applicable to your test, FDA recommends the following evaluations be performed and documentation kept on file. If applicable to your test, FDA recommends the following evaluations be performed prior to authorization and documentation kept on file.
You should evaluate the cybersecurity of your system to ensure user and patient safety in the intended use environment;10
You should complete validation of all systems and software to ensure that all functions of the system perform as labeled. For more information on system validation please see the following FDA guidance documents and resources:
[If you are introducing a system onto the market which has not been previously reviewed by the FDA, please describe how you addressed basic safety hazards such as electrical hazards (e.g., electrical shock to the operator and/or patient), fire hazards, and mechanical hazards.] We recommend that you consult the general requirements for basic safety, as indicated in International Electrotechnical Commission (IEC) 60601-1 (Medical electrical equipment – Part 1: General requirements for basic safety and essential performance). IEC 60601-1 is a standard that specifies the general requirements for basic safety and essential performance. IEC 60601-1 defines basic safety as freedom from unacceptable risk directly caused by physical hazards when medical electrical equipment is used under normal condition and single fault condition.
Electromagnetic Compatibility (EMC) Testing (if applicable):
We recommend that EMC testing be conducted on any assay that uses a battery or power source. [Please provide FDA with any standards that were followed for EMC testing.] We recommend that you perform EMC testing according to the International Electrotechnical Commission (IEC) 60601-1-2 Edition 4.0:2014. [If you perform EMC testing to a different standard or use alternate methodologies to evaluate EMC, please provide a test plan, test report, acceptance criteria, and risk analysis to support your approach.]
Manufacturing and Testing Capabilities:
[Briefly describe current sample throughput testing capacity, the total time required to perform the test (from clinical sample collection to result), and the number of tests that can be performed per day (8-hour shift), excluding controls and calibrator, as applicable. Please provide the number of kits you can manufacture per day/week for distribution in the United States.]
Distribution Plan:
The product will be distributed by [please describe the distribution plan for the product and list all current US distributors].
Reagent Stability:
[Briefly describe the stability test plan for test reagents and include any accelerated stability information, if available.] Real time reagent stability studies generally do not need to be completed at the time of EUA issuance; however, the study design should be agreed upon during interactive review and the stability studies started immediately following authorization, if not before. In the absence of real-time stability data, initial reagent stability claims should not exceed four to six months. Expiration dates can be extended once real-time data becomes available. You should consider the following recommendations when designing your stability study:
For EUAs, you may follow the current FDA recognized Clinical Laboratory Standards Institute (CLSI) Standard EP25 – Evaluation of Stability of In Vitro Diagnostic Reagents; Approved Guideline when evaluating the suitability of stability study designs. If you are planning to pursue clearance or approval for your device, we recommend discussing with FDA in more detail your stability design to facilitate potential use of the EUA data in your regular premarket submission.
For all the stability evaluations, you should include your external positive and negative controls and at least one sample, which should be prepared by spiking negative clinical matrix at an analyte concentration of 3-5x LoD of inactivated SARS-CoV-2, not recombinant protein. Please note that use of the positive controls alone is not recommended for reagent stability evaluation because controls are usually formulated at a moderate positive level.
If you are using multiple clinical sample types in which similar LoDs are determined, you should use the most challenging clinical matrix for this study.
You should evaluate at least 5 replicates and, if available, 3 different lots of reagents.
You should design your study to provide data for a timeframe that is about 10% longer than the one to be authorized. For example, 18 months should be supported by stability data out to 20 months and 7 days should include stability data out to 8 days.
FDA considers 15-30°C to represent room temperature conditions. Ideally, you should evaluate stability at both 15°C and 30°C; however, for the purposes of the EUA evaluation, 30°C is generally acceptable as it represents the worst-case scenario.
Unopened Kit Shelf-Life Stability:
You should evaluate real-time kit stability studies with unopened kits stored at the claimed storage temperature for your test.
Accelerated stability evaluations for unopened kits can be included for EUA requests to support shelf-life claims up to six months while the real-time studies are on-going. However, please note real-time stability data is generally needed to support regular pre-market submissions.
Unopened Kit Shipping Stability: You should evaluate the anticipated handling and shipping times and temperatures expected for unopened kits under different temperature conditions (e.g., summer, winter). The recommended summer profile is storage at 40oC for 8 hours and then 22oC for 4 hours and the recommended winter profile is -10oC for 8 hours and then 18oC for 4 hours.
In-use/Opened Kit Stability: Depending on your device, your stability study design should also support in-use stability of the kit reagents once the kit has been opened, e.g., storage at 2-8°C for 7 days. This includes on board stability once reagents have been placed on the instrument (if applicable).
Inverted stability (if applicable): Study should support stability for kits if stored inverted or in the wrong orientation.
Freeze-thaw Stability: If you recommend aliquoting the reagents to meet the end-users needs, following the initial thaw this recommendation should be supported by a freeze-thaw stability study, including the specific number of allowed freeze-thaw cycles.
FDA recommendations for analysis of real time stability studies are as follows:
Baseline of the study (t=0 of stability study) should not exceed one month from production;
Clear baselines should be described (e.g., one month from production) for each stability claim under each study;
Claims should be determined based on regression analysis. Any %change (%shift) from time zero (baseline) should be calculated between the target claim and the zero-time as (Ttest-Tbaseline)/ Tbaseline*100 with 95% confidence interval (CI) using the regression equation obtained from plotting the mean values. When formulating your acceptance criteria for evaluating the shift from baseline, you should consider the reproducibility of your device. Generally, the shift at the target claim due to storage cannot exceed 10-15%. The target stability is the next to last tested point that was within +/- 10% of time zero; and
Acceptance criteria may differ depending on the reproducibility of your device, the distribution of analyte concentration expected in samples from the intended use population, and the risk of false results to public health.
Antibodies:
As the pandemic progresses, FDA is gathering publicly available sequence data from the GISAID.15 We are currently monitoring the presence of SARS-CoV-2 variants that may contain amino acid changes within the protein sequences captured by anti-SARS-CoV-2 antibodies used in authorized antigen tests. As part of your EUA request, we request that you provide the following:
[A description of the anti-SARS-CoV-2 antibodies used in your test, including whether they are polyclonal or monoclonal.
The specific amino acid sequence(s) (including amino acid position numbers relative to the SARS-CoV-2 target) of the immunogen used to generate the anti-SARS-CoV-2 antibodies used in your test to detect SARS-CoV-2 antigen(s).
A description of how the immunogen was generated (e.g., synthetic peptide, recombinant protein, etc.).
A description of the epitope(s) (if known), including whether the epitope is linear or conformational, recognized by the anti-SARS-CoV-2 antibodies used in your test to detect the SARS-CoV-2 antigen(s).]
J. PERFORMANCE EVALUATION
The following validation studies should be performed to support your EUA request. Please note that, particularly for new technologies, FDA may request additional studies so we can adequately assess the known and potential risks and benefits associated with the candidate test. [For each validation study, you should provide a study protocol that includes a detailed, step-by-step description of how samples were prepared and how testing was conducted. You should also include complete study line data in an Excel-compatible format for all validation studies. The line data should present each replicate with the final antigen test result per the tests result interpretation. If your device includes an analyzer with a numeric output [(e.g., fluorescence, signal to cut-off ratio (S/Co)], you should include the analyzer values for each replicate].
All validation studies should be conducted with inactivated virus, not recombinant protein.
Limit of Detection (LoD) - Analytical Sensitivity:
You
should determine the LoD of the candidate
test
utilizing
the entire test system from sample preparation and extraction to
detection. We recommend spiking quantified
virus
(e.g., heat
treated, chemically modified, or
irradiated
virus) into real clinical matrix (e.g., nasal, or nasopharyngeal (NP)
swabs, bronchoalveolar
lavage (BAL)
fluid, sputum, etc.). The use of recombinant antigen is not
recommended for the LoD determination. Respiratory
sample
collected
from SARS-CoV-2 negative individuals can be used as clinical matrix.
If VTM is indicated for use, you should spike swabs with virus prior
to immersing into VTM. Collection media without clinical matrix or
collection kits that
were not used to collect a clinical sample
are generally not considered real clinical matrix.
FDA
recommends
that preliminary LoD
be determined by testing
a 2-3-fold dilution series of 3 replicates per concentration, and
then confirmed
with
20 replicates of the
concentration determined to be the preliminary LoD.
For purposes of this document, the preliminary LoD is the lowest
concentration that gives positive results 100% of the time and the
final LoD is the lowest concentration at which 19 of 20 replicates
are positive. The
preliminary LoD studies should include at least one concentration
that does not yield 100% positive results. If
multiple matrices are intended for clinical testing, you should
include the results from one representative of each indicated
clinical matrix to FDA. The
most challenging matrix of the claimed matrices should be tested. For
example, if
testing respiratory samples
(e.g., sputum, BAL, NP swabs, etc.), please submit results from one
upper respiratory matrix and one lower respiratory matrix. FDA
considers NP swabs with and without your claimed VTM to be the most
challenging upper respiratory matrix and sputum to be the most
challenging lower respiratory matrix. If claiming other sample
types (saliva, etc.), we recommend that you establish your LoD in
each matrix, with and without transport media, as applicable. FDA
recommends that you follow the most current version of the
CLSI
EP17
“Evaluation
of Detection Capability for Clinical Laboratory Measurement
Procedures.”
[Please provide your complete LoD study protocol that includes a step-by-step description of how samples were prepared and tested with your device, the specific viral material used to assess the LoD (e.g., irradiated virus), and the LoD (with appropriate units) for your assay. Please provide the line data for the LoD study in an Excel-compatible format. If the assay includes use of an analyzer or application to generate test results, please include the analyzer value for each test replicate.]
LoD studies determine the lowest detectable concentration of SARS-CoV-2 at which approximately 95% of all (true positive) replicates test positive. The LoD was determined by limiting dilution studies using characterized [please describe samples used in the study, e.g., viral stocks].
[List/describe the following in this section:
Titers and strains of the SARS-CoV-2 stocks used for the LoD study and how the organism stocks were prepared and how the titers were determined.
The dilution factor and number of serial dilutions of the characterized SARS-CoV-2 that were tested to determine the LoD.
The starting concentration, dilution factor used to reach target concentration, the volume of negative matrix with inactivated SARS-CoV-2 spiked onto each swab in your LoD study, and the type of dilutant used (e.g., Phosphate Buffered Saline (PBS), saline, etc.) to prepare each replicate in your LoD study. Please note that it is generally not appropriate to prepare samples with your assay reagents (e.g., extraction buffer) nor is it generally appropriate to dilute clinical matrix in VTM if the test is not indicated for use with VTM given that FDA has observed performance variability with use of certain VTMs and thus, the use of VTM may adversely impact the performance.]
Serial dilutions of the characterized SARS-CoV-2 made in clinical matrix obtained from individuals who tested negative for SARS-CoV-2 were then tested in [number of replicates] replicates. The lowest concentration at which all [number of replicates] replicates were positive was treated as the tentative LoD for each test. The LoD of each test was then confirmed by testing [number of replicates (at least 20 recommended)] with concentrations at the tentative limit of detection. The final LoD of each test was determined to be the lowest concentration resulting in positive detection of [number of positive replicates (at least 19 out of 20 replicates)]. [Include analysis of LoD results, indicating the final LoD for each test].
Note: The LoD range finding study should include at least one concentration that achieves 95% detectability of replicates and at least one concentration that achieves less than 95% detectability. Replicates should be interpreted per the result interpretation of your test.
Inclusivity (analytical reactivity):
Mutations in the SARS-CoV-2 genome have been identified as the virus has spread. A mutation is an individual genetic change in a SARS-CoV-2 virus sequence when compared with a reference sequence such as Wuhan-Hu1 or USA-WA1/2020. A new virus variant of SARS-CoV-2 has one or more mutations that differentiate it from the wild type or predominant virus variants already circulating in the general population. Variants of SARS-CoV-2 are identified by genomic sequences that contain mutation(s) in the RNA genome, which could result in amino acid substitutions, insertions, and/or deletions in viral proteins. Different variants can result in different phenotypes (e.g., a difference in antigenicity, transmissibility, or virulence). Viral mutations and viral variants could result in altered immunogenicity relative to the originally isolated virus, which could impact the performance of antigen tests.
Test developers should monitor new and emerging viral mutations and variants that could impact antigen test performance on an ongoing basis. This includes assessing the prevalence of viral mutations in sequence databases, as mutations observed in these databases at a significant frequency may signify that the mutation is present in an increasing proportion of infected individuals in the U.S. FDA currently considers a significant frequency to be greater than 5% (when considering at least 2000 sequences over a recent period of time, such as the past week, month, or quarter). Monitoring should also include identifying if there are multiple credible reports indicating that a given viral variant (which may have one or more mutations) has the potential to increase virulence, increase transmission, or otherwise increase the public health risk. FDA recommends monitoring on at least a monthly basis in light of the rate of occurrence of mutations and variants and the importance of assessing their impact.
For any viral mutations and variants that are identified as prevalent and/or clinically significant as described above, you should assess whether the resulting predicted amino acid change(s) in the viral proteins are critical to your test design. If the mutations are found to be critical to your test design, such mutations and variants should be evaluated using clinical (or contrived, as available and as appropriate) samples to assess the impact of the mutation or variant on your test’s performance. The aggregate impact of the mutations should not reduce the clinical performance of the test by 5% or more or decrease the clinical performance point estimates for the test below the clinical performance recommendations described in Section J(10).16
Please see the FDA guidance document “Policy for Evaluating Impact of Viral Mutations on COVID-19 Tests” for additional discussion regarding monitoring the impact of genetic variants on antigen diagnostic tests.
FDA also has ongoing monitoring efforts and may identify a viral mutation or variant as clinically significant for which testing with clinical (or contrived, as available and as appropriate) samples would be recommended to assess the impact of the mutation or variant on the performance of your test.
[Please provide your plan for monitoring for new and emerging SARS-CoV-2 viral mutations and variants on an ongoing basis and for assessing the impact of mutations and variants that have been identified as prevalent and/or clinically significant on the performance of your assay over time.]
[For mutations and variants that have been identified as prevalent and/or clinically significant as part of ongoing monitoring at the time of your EUA request, please provide information on the potential impact of the mutation(s) and variants on your test’s performance or explain how the risk associated with the unknown performance of your device in samples from individuals with the variant(s) can be adequately mitigated.]
Cross-reactivity (Analytical Specificity):
Cross-reactivity studies are performed to demonstrate that the test does not react with related pathogens, high prevalence disease agents, and normal or pathogenic flora that are reasonably likely to be encountered in the clinical sample. We recommend that the organisms in the table below are wet-tested in negative clinical matrix in three replicates; please contact FDA if you are unable to obtain specific organisms to discuss potential options and labeling mitigations. In silico analyses may be appropriate for certain organisms (see table below). We recommend using concentrations of 106 CFU/ml or higher for bacteria and 105 pfu/ml, or TCID50/mL (tissue culture infective dose) or higher for viruses. We recommend assessing potential cross-reactivity of the organisms listed in the table below, as applicable to the claimed sample type. If you are claiming an alternative matrix not listed below, please contact FDA to discuss the list of microorganisms recommended for testing.
[Please provide your complete cross-reactivity protocol, including a step-by-step description of how samples were prepared (e.g., starting concentration, dilution factor used to reach target concentration, volume of organism suspension, volume of clinical matrix, etc.) and tested with your device, the specific materials used to assess cross-reactivity and where these materials were obtained. Please include the Certificates of Analysis for each microorganism that is tested, or equivalent information (e.g., the culture protocol, lot number, manufacturing date, viral strain, a description of viral inactivation, pre-inactivation titer, and pre-inactivation sterility for viral isolates, etc.). For bacterial isolates, information may also include the isolate source, method for identification, number of passages, microbiological features, or other information. Please provide the line data for the cross-reactivity study as part of your request, in an Excel-compatible format. If the assay includes use of an analyzer or application to generate test results, please include the analyzer value with each test replicate.]
Recommended List of Organisms to be Analyzed in silico and by Wet Testing for All for Respiratory Samples
High priority pathogens from the same genetic family |
High priority organisms likely present in respiratory samples |
Human coronavirus 229E (Wet-testing) |
Adenovirus (e.g., C1 Ad. 71) (Wet-testing) |
Human coronavirus OC43 (Wet-testing) |
Human Metapneumovirus (hMPV) (Wet-testing) |
Human coronavirus NL63 (Wet-testing) |
Parainfluenza virus 1-4 (Wet-testing) |
MERS-coronavirus (Wet-testing) |
Influenza A & B (Wet-testing) |
SARS-coronavirus (Wet-testing) |
Enterovirus (Wet-testing) |
Human coronavirus HKU1 (In-silico (protein blast)) |
Respiratory syncytial virus (Wet-testing) |
|
Rhinovirus (Wet-testing) |
|
Haemophilus influenzae (Wet-testing) |
|
Streptococcus pneumoniae (Wet-testing) |
|
Streptococcus pyogenes (Wet-testing) |
|
Candida albicans (Wet-testing) |
|
Pooled human nasal wash – representative of normal respiratory microbial flora (Wet-testing) |
|
Bordetella pertussis (Wet-testing) |
|
Mycoplasma pneumoniae (Wet-testing) |
|
Chlamydia pneumoniae (Wet-testing) |
|
Legionella pneumophila (Wet-testing) |
|
Staphylococcus aureus (Wet-testing) |
|
Staphylococcus epidermidis (Wet-testing) |
|
Mycobacterium tuberculosis (In-silico (protein blast))* |
|
Pneumocystis jirovecii (PJP) (In-silico (protein blast))* |
*M. tuberculosis and P. jirovecii are applicable to lower respiratory matrices only (e.g., BAL, sputum, etc.).
High Priority Organisms Likely Present in Saliva Samples Recommended List of Organisms to be Analyzed in silico and by Wet-Testing for Saliva Samples**
Other high priority pathogens from the same genetic family |
High priority organisms likely in the circulating area |
Human coronavirus 229E (Wet-testing) |
Adenovirus (e.g., C1 Ad. 71) (Wet-testing) |
Human coronavirus OC43 (Wet-testing) |
Human Metapneumovirus (hMPV) (Wet-testing) |
Human coronavirus NL63 (Wet-testing) |
Parainfluenza virus 1-4 (Wet-testing) |
MERS-coronavirus (Wet-testing) |
Influenza A & B (Wet-testing) |
SARS-coronavirus (Wet-testing) |
Rhinovirus (Wet-testing) |
Human coronavirus HKU1 (In-silico (protein blast)) |
Respiratory syncytial virus (Wet-testing) |
|
Herpes Simplex Virus-1 (HSV-1) (Wet-testing) |
|
Epstein-Barr Virus (EBV) (Wet-testing) |
|
Cytomegalovirus (CMV) (Wet-testing) |
|
Moraxella catarrhalis (Wet-testing) |
|
Porphyromonas gingivalis (Wet-testing) |
|
Bacteroides oralis (Wet-testing) |
|
Nocardia sp. (Wet-testing) |
|
Streptococcus mutans (Wet-testing) |
|
Streptococcus mitis or other Strep viridans (Wet-testing) |
|
Eikenella sp. (Wet-testing) |
|
Neisseria sp. (Wet-testing) |
|
Candida albicans (Wet-testing) |
|
Pseudomonas aeruginosa (Wet-testing) |
|
Staphylococcus epidermis (Wet-testing) |
|
Streptococcus salivarius (Wet-testing) |
**These organisms should be analyzed/tested in addition to the ones included in the immediately preceding table.
Microbial Interference Studies:
If cross-reactivity is not observed between your assay and any of the microorganisms listed above, you should conduct a microbial interference study. A microbial interference study demonstrates that false negatives will not occur when SARS-CoV-2 is present in a sample with other microorganisms. You should prepare contrived samples in your most challenging claimed matrix with SARS-CoV-2 and common organisms found in that matrix. You should provide a list of common pathogens or commensal organisms for your most challenging matrix as part of your request.
If applicable, microbial interference should be evaluated using samples spiked at a low (2-3x LoD) SARS-CoV-2 concentration and a high interferent level (i.e., microorganisms), to represent the worst-case scenario, with a minimum of three replicates. The interferent microorganisms can be tested individually or as a pool (of 4-5); each microorganism should be tested individually if that pool shows interference. If you plan to claim both upper and lower respiratory matrices, the study should be performed in the most challenging respiratory matrix (i.e., sputum). If interference is observed at the level tested, an additional titration study should be performed to determine the highest microorganism interferent level your test can tolerate.
[Please provide your complete microbial interference study protocol, including a step-by-step description of how samples were prepared (e.g., starting concentration, dilution factor used to reach target concentration, and volume of organism suspension for both inactivated SARS-CoV-2 and microbial interferent, volume of clinical matrix, etc.) and tested with your device, the specific materials used to assess microbial interference and where these materials were obtained. Please provide the line data for the microbial interference study in an Excel-compatible format. If the assay includes use of an analyzer or application to generate test results, please include the analyzer value with each test replicate.]
Endogenous/Exogenous Interference Substances Studies:
The extent of testing for interference substances depends on the matrix that is indicated for the candidate test, as well as on the technology of the candidate test. We recommend testing the following substances listed in the tables below, as applicable based on the indicated matrices, with and without inactivated virus at 2-3x LoD in three replicates for each substance. Please contact FDA if you have questions about appropriate study designs.
List of Potential Interfering Substances Recommended for Testing When the Candidate Test is Indicated for Respiratory Samples
Potential Interfering Substances |
Concentration |
Whole Blood |
4% |
Mucin |
0.5% |
Chloraseptic (Menthol/Benzocaine) |
1.5 mg/mL |
Naso GEL (NeilMed) |
5% v/v |
CVS Nasal Drops (Phenylephrine) |
15% v/v |
Afrin (Oxymetazoline) |
15% v/v |
CVS Nasal Spray (Cromolyn) |
15% v/v |
Zicam |
5% v/v |
Homeopathic (Alkalol) |
1:10 dilution |
Sore Throat Phenol Spray |
15% v/v |
Tobramycin |
4 μg/mL |
Mupirocin |
10 mg/mL |
Fluticasone Propionate |
5% v/v |
Tamiflu (Oseltamivir Phosphate) |
5 mg/mL |
List of Potential Interfering Substances Recommended for Testing When the Candidate Test is Indicated for Saliva and Oral Samples
Substance |
Concentration |
Cepacol Lozenges (benzocaine/menthol) |
3 mg/mL |
Cough drops (Dextromethorphan HBr) |
|
Robitussin |
|
Chloroseptic Sore Throat spray (Phenol, Glycerin) |
5% v/v |
Emergen-C (Zinc, Magnesium, Riboflavin, Vitamin C) |
|
Crest/Listerine Mouthwash (Eucalyptol, menthol, Methyl Salicylate, Thymol) |
5% v/v |
Act dry mouth lozenges (Isomalt, xylitol, Glycerin) |
|
Toothpaste (Colgate) |
0.5% v/v |
Nyquil (Acetaminophen, Doxylamine succinate, Dextromethorphan HBr) |
|
Mucin: bovine submaxillary gland, type I-S |
2.5 mg/ml |
Human Genomic DNA |
10 ng/μl |
Vaseline (Petroleum Jelly) |
|
Nicotine |
0.03 mg/ml |
Alcohol (Ethanol) |
5% |
White blood cells/Leukocytes |
1 to 5x106 cells/mL |
Whole Blood |
2.5% |
[If a concentration is not listed in the table above, please determine an appropriate concentration and provide the scientific justification supporting your proposed concentration as part of your EUA request.]
Biotin Interference:
If your assay uses a biotin/anti-biotin capture system, biotin interference testing should be conducted. False negative results may occur in patients who have indicated or whose clinical status or history would indicate they are currently taking high doses of biotin. We recommend testing up to 3,500 ng/mL with and without SARS-CoV-2 at 2-3x LoD in your most challenging clinical matrix. If biotin interference is observed, please provide an appropriate labeling limitation in your instructions for use.
[Please provide your detailed biotin interference protocol, including a step-by-step description of how samples were prepared and tested with your device, and all study results in an Excel-compatible format, with analyzer values, if applicable.]
High-dose Hook Effect:
A high-dose hook effect refers to the false negative result which can be seen when very high levels of target are present in a tested sample. We recommend you conduct studies to evaluate if a hook effect occurs by testing increasing antigen concentrations and, if applicable, indicate the concentration which begins to affect assay performance. [Please provide a detailed study protocol, including step-by-step description of how you prepared and tested each replicate, and provide all study data in an Excel compatible format, with analyzer values, if applicable.]
Testing should be conducted to demonstrate sample stability throughout the real-world conditions in which they are collected and tested, according to your instructions for use. When the test is intended to be performed on the sample immediately or shortly after obtaining the sample, sample stability testing could be relatively short (i.e., 2 hours at room temperature) and conducted with contrived samples at 3x LoD using inactivated virus spiked into negative clinical matrix. If you intend to test retrospective clinical samples in your clinical study that have been frozen, you should also conduct fresh versus frozen studies to support use of these samples.
LoD Target Level |
Number of Samples |
3-5x LoD |
10 |
1-2x LoD |
30 |
Negative |
10 |
Total |
50 |
[Please provide a complete sample stability protocol, including a detailed, step-by-step description of how you prepared and tested each replicate, and provide all study data in an Excel-compatible format, with analyzer values, if applicable.]
VTM/UTM Equivalency:
Each brand of validated transport media should be listed in your intended use statement and validated during your clinical and analytical validation studies. FDA has observed significant cross-reactivity with different brands and types of VTM, which has resulted in erroneous patient results. Without validating and specifying each type of VTM/UTM intended for use with your device, we cannot determine if your device is fully validated to assess the risk of erroneous results due to cross-reactivity with affected types of VTM/UTM. Once an EUA has been granted, additional brands or types of VTM can be added with a VTM equivalency study. An appropriate VTM equivalency study for most types of VTM would test 5 replicates at 2x LoD, 5 replicates at 5x LoD and 10 negative replicates for three lots of each claimed VTM (60 total replicates per VTM). Each replicate should be prepared in negative clinical matrix. For types of VTM with known cross-reactivity issues, additional negative replicates may be requested.
[Please provide a complete VTM equivalency protocol, including a detailed, step-by-step description of how you prepared and tested each replicate, and provide all study data in an Excel-compatible format, with analyzer values, if applicable.]
Clinical Evaluation for Patients Suspected of COVID-19:
FDA recommends conducting prospective, blinded, randomized clinical agreement trials with at least 30 positive samples and 30 negative natural clinical samples from patients who represent your intended use population (e.g., symptomatic within X days of symptom onset, asymptomatic individuals, etc.). The number of negative samples may vary according to the disease prevalence at the time of your study. Evaluations with contrived clinical specimens are inadequate to support the clinical performance of an antigen test at this time.
If you seek authorization for multiple sample types, each sample type should be evaluated. Please note that samples with and without VTM are considered two distinct types of samples. FDA has observed significant cross-reactivity with different brands and types of VTM, which has resulted in erroneous patient results. As a result, FDA does not recommend VTM for use with lateral flow tests. Use of VTM should be limited to tests indicated for use with moderate and high complexity laboratory use as VTM is intended for transport of specimens to these settings.
Samples from each individual should be evaluated with the candidate test and an authorized reverse transcription polymerase chain reaction (RT-PCR) test which uses a chemical lysis step followed by solid phase extraction of nucleic acid (e.g., silica bead extraction) and reports a cycle threshold (Ct) value. The comparator test should be one of the more sensitive RT-PCR assays authorized by FDA. We encourage you to review the results from the FDA SARS-CoV-2 Reference Panel17 and contact us to discuss your choice of comparator test. Evaluations with the comparator test should be conducted per the authorized instructions for use. Please contact FDA if you are considering using a modified configuration of an authorized RT-PCR assay.
When collecting samples, the standard of care sample (i.e., the sample used for clinical and not investigational purposes) should always be collected first, including when the comparator test is also the standard of care. If the comparator test is not the standard of care, swabs taken from the same anatomical area for the comparator test and candidate test (e.g., mid-turbinate swabs compared with NP swabs, etc.) should be randomized to ensure that bias is not introduced due to an unequal distribution of viral materials. When two distinct anatomical sites are being assessed, it is not necessary to randomize sample collection order (e.g., saliva compared to NP swabs). All clinical samples tested in your study should be evaluated in accordance with the candidate test’s proposed diagnostic algorithm (i.e., tested using the procedure in the instructions for use), including retesting when appropriate. To minimize the occurrence of discordant results due to biological variability, both samples should be collected within a short time period (e.g., within the same healthcare visit). Samples should be tested in a blinded fashion, e.g., positive and negative samples should be presented to the end user in a blinded fashion. The end user should also be blinded to the results of any comparator method testing.
FDA recommends establishing a discordant analysis plan prior to your clinical study. Discordant samples should be tested with a second EUA authorized RT-PCR test that has also demonstrated high sensitivity, and which uses a chemical lysis step followed by solid phase extraction of nucleic acids (e.g., silica bead extraction). Results from a discrepant analysis should not be included in the calculation of negative percent agreement (NPA) and positive percent agreement (PPA) but may be added to the performance table as a footnote.
You may consider use of an enrichment strategy in which individuals with a known COVID-19 infection status are invited to participate in your clinical evaluation study. If using an enrichment strategy, you should carefully consider how you will randomize and blind operators to the participant’s infection status and minimize potential bias. Data from an enriched study design should represent the full range of viral loads, with both low and high positives samples. Therefore, it is not appropriate to use a rapid antigen test to enrich for asymptomatic participants, as it will select for strong positive samples. Please contact FDA to discuss any alternative study designs or enrichment strategies.
As the lower sensitivity of many antigen tests may not support use in all individuals suspected of infection, the number of days post symptom onset should be captured for all clinical samples. If you believe your test may have appropriate performance for all individuals suspected of infection, please contact FDA to discuss alternative clinical study recommendations and the necessary supportive clinical data.
Samples from individuals that are not indicated for testing as part of the proposed intended use statement should be excluded from the primary data analysis. If insufficient descriptive information is available (such as days post symptom onset), then the sample should be excluded.
You may submit your EUA request with results from only the first five prospective clinical samples if you have also conducted a study with retrospective clinical samples. Retrospective clinical samples should be randomized and tested blindly at your clinical study sites. All positive retrospective clinical samples should be reflective of the natural distribution of SARS-CoV-2 viral loads. Approximately 10-20% of the clinical samples should be low positives, as has been observed in other sequentially enrolled clinical studies. Low positives are defined for purposes of this document as samples in which any gene target is within 3 cycle thresholds (Ct’s) of the mean Ct count at the comparator test’s LoD. If a retrospective study is leveraged for authorization, the completed prospective study would be provided post-authorization.
Studies involving clinical samples (human specimens) conducted in support of an EUA request are subject to applicable requirements for Institutional Review Board (IRB) review and approval and informed consent (see 21 CFR parts 50, 56, and 812). FDA’s policy regarding informed consent requirements for certain studies using leftover, de-identified samples is outlined in the FDA guidance “Guidance on Informed Consent for In Vitro Diagnostic Device Studies Using Leftover Human Specimens that are Not Individually Identifiable.”18
Candidate tests should demonstrate a minimum sensitivity of ≥ 80% for all sample types submitted. For less sensitive tests, you may consider leveraging a serial testing strategy and evaluate the candidate test’s cumulative performance rather than its one-time test performance. If you are proposing serial testing as a mitigation for a less sensitive candidate test, you should provide data to support the cumulative clinical performance ≥ 80% sensitivity as well as detailed instructions for serial testing in the package insert, including the recommended testing interval, that are supported by your clinical data. You should also discuss how you will ensure compliance with serial testing post-authorization, such as multi-test packs, software applications, or other mitigations. Additional post-authorization studies may be necessary to assess the success of your proposed mitigations.
[Please describe the clinical study used to evaluate the clinical performance of the test. including the following:
[The names and locations of the collection and testing sites, number of samples collected at each site, and number of operators used to run your assay at each site;
Enrollment criteria (inclusion/exclusion criteria);
The name of the comparator test, including a detailed laboratory protocol for performing the comparator test, including the platform and extraction kit;
A detailed description of the patient population at each site;
The sample matrix(ces) tested for both the candidate test and comparator test;
A detailed description of how patients were enrolled and tested;
A detailed description of the method of randomization;
A detailed description of the method of blinding;
The technique and collection device(s), including transport media, used to obtain clinical samples. All clinical samples tested in your study should be evaluated in accordance with the candidate test’s proposed diagnostic algorithm, including retesting when appropriate;
A detailed description of how samples were collected, transported, stored, and tested with the candidate test and the comparator test; and
11. A detailed description of the order in which swabs were collected.]
[Please provide the following study data in an Excel compatible file:
Sample type for the candidate test
Sample collection date and time for the candidate test
Sample testing date and time for the candidate test
VTM type, as applicable, for the candidate test and candidate test
Candidate test result with the analyzer or reader value
Sample type for comparator test
Sample collection date and time for comparator test
Sample testing date and time for RT-comparator test
Name of comparator test
Comparator test results (+/-)
Comparator test value results (Ct values)
Number of days post-onset of patient symptoms
Clinical Evaluation for Screening Individuals Without Symptoms or Other Reasons to Suspect COVID-19:
The recommendations below reflect FDA’s current thinking. The study design and recommendations may change as additional information becomes available regarding asymptomatic infections, including but not limited to viral titer dynamics and transmission rates in this population.
If you seek claims for screening individuals without symptoms or other reasons to suspect COVID-19, FDA recommends that you conduct a prospective clinical study in asymptomatic individuals free of any symptoms of SARS-CoV-2 infection for at least two weeks prior to enrollment and testing. If an individual previously tested positive, there should be at least two weeks from the time of last positive test prior to enrollment and testing. Asymptomatic individuals who are suspected of COVID-19 (i.e., via exposure) should be excluded. As part of your clinical study protocol and data, you should document how you screened and confirmed that all enrolled individuals were asymptomatic and consistent with your proposed intended use.
You should follow the clinical study recommendations listed above (i.e., 30 symptomatic positive and 30 negative samples), except that you should enroll at least 20 positive asymptomatic individuals to collect unique samples. It may also be appropriate to present the results from 10 positive samples from asymptomatic individuals prior to EUA authorization, provided data from symptomatic individuals are also submitted and analysis of Ct values demonstrates reasonably similar distribution of viral loads. The remainder of the 20 positive clinical samples collected from unique asymptomatic individuals can be provided post-authorization and incorporated as a condition of authorization.
Developers may also refer to the Supplemental Template for Developers of Molecular and Antigen Diagnostic COVID-19 Tests for Screening with Serial Testing19 for additional options when seeking a screening indication with serial testing when a clinical evaluation with symptomatic patients suspected of COVID-19 infection by their healthcare providers has been performed.
Studies to Support Point of Care (POC) Use, as applicable:
[If the device is intended for POC testing, please provide a detailed study description and data to demonstrate that non-laboratory healthcare providers can perform the test accurately in the intended use environment.] Your studies to support a POC claim should include the following: (1) a POC clinical evaluation including use of appropriate sites and test users, (2) supplemental POC samples, and (3) POC flex studies. For more details, please see each section below.
Clinical Evaluation:
The clinical study design should reflect how the test will be used in clinical practice. It is expected that a test with “POC” designation will be widely used in CLIA waived medical facilities (e.g., physician office, outpatient clinic, emergency room (ER)), but also in less traditional settings (e.g., tents, schools, etc., with health care provider oversight of testing) where health care providers are present.
Please see section J(10), for recommendations regarding clinical validation studies. The clinical evaluation study recommendations from section J(10) are applicable to POC clinical evaluation studies. Please note that all elements of the clinical evaluation study for a candidate test intended for POC use should be conducted in an appropriate POC clinical study site (i.e., a CLIA waived site in the US). You may also send the samples for the EUA authorized RT-PCR comparator test to a central laboratory for testing if that is within the comparator test’s authorized intended use.
[Please include study data presented in an Excel-compatible format and include the same data elements outlined in section J(10).]
Sites and Test Users (Operators):
You should select one or two non-laboratory sites in the United States (U.S.) to assure that the operators are representative of intended operators in the U.S., e.g., doctor’s office, ER, outpatient clinic, drive-through testing facility, or another area in a medical facility outside the central laboratory where samples are collected and tested in real time. This would allow evaluation of the sample collection and handling, including addition into the sample port/well of the test, both of which may be significant sources of error. Four to six operators representing intended healthcare provider operators, but who are not laboratory trained (e.g., nurses, nursing assistants and doctors) should participate in the study. During the clinical study, operators should not be trained on use of the antigen test. Testing should be performed using only Quick Reference Instructions (QRI) - supplemental materials, such as a video or a mobile application that can be easily accessed by the user, are encouraged to be included with the proposed candidate test but should not be used during this study in order to mimic the worst-case scenario.
[Please provide the detailed individual replicate result data in an Excel-compatible formant and protocols for each of your studies, including:
The objective of the study;
Detailed test procedure;
Materials used;
A list of samples tested;
Results (presented in tabular format), including invalid results;
Conclusions;
Any appropriate mitigation measures (e.g., labeling changes, changes to test design, etc.); and
Operator background (e.g., education, training, experience, etc.)
As part of your EUA request, please include a table in which your study results are stratified by operator.]
Performance around LoD:
You should also conduct testing with contrived samples prepared with SARS-CoV-2 viral load near the LoD of the candidate test in clinical matrix. The testing should be conducted by untrained operators and should consist of 10 low positives (<2xLoD) and 10 negative samples per site. All contrived samples should be blinded and randomized and tested as part of the normal workflow of the POC clinical site. Each operator should test at least 3 low positive and 3 negative samples. These samples are intended to supplement, not replace, the clinical samples in your study. These samples may be used to demonstrate that each untrained operator has tested at least 3 positive and 3 negative samples.
[Please include a table in an Excel-compatible format in which your study results are stratified by operator.]
POC Flex Studies:
You should also conduct a thorough hazard analysis considering the main known sources of errors. Based upon your hazard analysis, you should conduct flex studies to evaluate the impact of errors, or out-of-specifications conditions, on the candidate test performance. Each sample should be prepared at 2xLoD in negative clinical matrix and should be evaluated in three replicates for each condition under evaluation. Flex studies can be conducted with trained operators at an internal testing site. Each study should be performed using a pre-defined study protocol that includes the following:
The objective of the study;
Detailed test procedure; and
Materials used.
Potential stress conditions include:
40°C and 95% room humidity (RH) (mimicking hot and humid climates);
Delay in sample testing or reading time;
Delay and/or disturbance in operational steps;
Sample volume variability;
Buffer volume variability;
Read Time variability; and
Other, as appropriate.
[Please provide a detailed, step-by-step description of how you prepared and tested each replicate and provide all study data in an Excel compatible format, with analyzer values, if applicable. Data for each sample evaluated (i.e., line data) should be provided. If erroneous results are observed during studies evaluating the robustness of the device, adequate mitigation(s) should be provided.]
Please see the Template for Developers of Molecular and Antigen Diagnostic COVID-19 Tests for Home Use20 for more in-depth flex study designs. Alternative sources of information on flex studies that may be appropriate for the candidate test can be found on the FDA CDRH website containing CLIA Waiver by Application Decision Summaries.21
If you are requesting an EUA for a multiplex respiratory panel, analytical and clinical evaluations for each target analyte should be included. We recommend considering the study designs and data summaries noted in the published EUA Summaries and Instructions For Use of authorized multiplex tests.
The validation needed to support an EUA may vary if the test platform was previously cleared by FDA, as noted below. The following analytical studies should be conducted, and data provided to the FDA for review:
Limit of Detection (Analytical Sensitivity)
Cross-Reactivity / Microbial Interference
Inclusivity / Analytical Reactivity, when different strains become available
Competitive inhibition (for analytes for which the test is indicated for use)
Interfering Substances Study (Endogenous and Exogenous)
Clinical Sample Stability
Reagent Stability testing protocol
Carry over/Cross-Contamination (if a new instrument/test not previously cleared/approved by the FDA is used with the candidate test)
Reproducibility and Repeatability (if a new instrument/test not previously cleared/approved by the FDA is used with the candidate test)
Fresh vs. Frozen - If you intend to submit data collected from testing archived frozen samples in support of your EUA, please conduct an analytical study to demonstrate that preservation of samples (e.g., by freezing at ≤-70°C) does not affect the accuracy of test results compared to freshly collected samples. See section J(7) for fresh vs. frozen study recommendations.
[If you are modifying a test that was previously authorized or cleared by FDA, you should present a side-by-side description of the two tests in which you compare all components and reagents, including a description of the reagents (including antibodies), volumes, concentrations, quantities, buffer components, etc., and any differences in instrumentation and software.]
For a multiplex candidate test that includes indications for Influenza A and/or Influenza B, you should establish the LoD on at least two strains of Influenza A and Influenza B. We recommend using one H1N1 post-2009 isolate and contemporary H3N2 isolate for Influenza A and a contemporary isolate of Yamagata and Victoria lineages for Influenza B.
A multiplex candidate test that includes Influenza A and/or B should also verify the analytical reactivity of the candidate test against the Centers for Disease Control and Prevention (CDC) human influenza panel to ensure adequate performance against currently circulating strains of influenza. Information on how to request this panel can be found at CDC’s “Request for CDC Influenza Virus Panel” website.22 If the CDC reference panel is not available, it may be appropriate to obtain the selected strains from other sample repositories for testing, provided that adequate documentation for each strain is included in your EUA request (i.e., Certificates of Analysis).
Clinical Performance: To evaluate the clinical performance of a multiplex respiratory panel, a prospective clinical study should be conducted as per the recommendations in section J(10). Considering the public health needs in the current emergency, a clinical evaluation study in support of the EUA request may be conducted at one US site testing positive and negative clinical samples. All of your clinical samples should include results from an EUA-authorized RT-PCR comparator test indicated for COVID-19 and an FDA cleared RT-PCR comparator test indicated for Influenza A, B, and/or other respiratory pathogens, in which 10-20% of the SARS-CoV-2 samples are low positive samples.
Multi-analyte Panels not Previously Cleared by the FDA
For devices that were not previously FDA-cleared for influenza or other respiratory pathogens, please conduct a prospective clinical study of at least 50 positive Influenza A samples, 30 positive samples from Influenza B or other respiratory pathogens and 30 negative samples. Each sample type for which the candidate test is indicated should be evaluated. If sufficient positive prospective samples were not collected during the clinical study, results may be supplemented with data from retrospective samples and an additional prospective clinical study may be conducted post-authorization. You should submit your EUA request with results from five prospective clinical samples, if you have conducted a study with retrospective clinical samples.
A post-authorization prospective clinical study included as a condition of authorization generally should include a minimum of three sample collection sites and three testing sites, prospectively enrolling patients with general respiratory symptoms. In some cases, it may be appropriate to conduct a prospective clinical study in the Southern Hemisphere during the typical influenza/respiratory season there to increase the likelihood of obtaining a sufficient number of positive samples (e.g., for influenza at least 50 positive Flu A and 30 positive Flu B samples) in a timely fashion. Please contact FDA prior to conducting studies outside of the U.S.
Addition of SARS-CoV-2 to previously FDA-cleared Multiplex Respiratory Panels
If your device has been previously FDA-cleared for influenza or other respiratory pathogens and no modifications have been made to your previously FDA-cleared analytes, you should confirm that the LoD for the previously cleared pathogens is unchanged due to the modification by conducting side-by-side testing of 3-5 replicates of serially diluted viruses with the original and modified versions of the candidate test. You should also test at least 10 positive and 10 negative clinical samples of each type of analyte for which the candidate test was previously cleared. You should perform a competitive inhibition study with clinically relevant titers of each analyte in the panel (viruses 105 PFU/mL, bacteria 106 CFU/mL). All studies to validate your test for the detection of SARS-CoV-2 should be conducted, as described above.
[If you are modifying a test that was previously authorized or cleared by FDA, you should present a side-by-side description of the two tests in which you compare all components and reagents, including a description of the reagents (including antibodies), volumes, concentrations, quantities, buffer components, etc., and any differences in instrumentation and software.]
K. UNMET NEED ADDRESSED BY THE PRODUCT
This section will be completed by FDA.
L. APPROVED/CLEARED ALTERNATIVE PRODUCTS
There is no adequate, approved, and available alternative to the emergency use of the product.
M. BENEFITS AND RISKS:
This section will be completed by FDA.
FACT SHEET FOR HEALTHCARE PROVIDERS AND PATIENTS:
During review, FDA will make available Fact Sheet templates. See examples for authorized tests on our website.23
INSTRUCTIONS FOR USE/ PROPOSED LABELING/PACKAGE INSERT:
[You should include Instructions for Use, Box Labels, Vial Labels, and any other proposed labeling.]
P. RECORD KEEPING AND REPORTING INFORMATION TO FDA:
As allowed by Section 564(e) of the FD&C Act, FDA may require certain conditions as part of an EUA. FDA generally includes the following record keeping and reporting information requirements in the EUA.
[Test Developer name] will track adverse events and report to FDA under 21 CFR Part 803. A website is available to report on adverse events, and this website is referenced in the Fact Sheet for Health Care providers as well as through the [Test Developer name] Product Support website: [Include link to Test Developer’s Website]. Each report of an adverse event will be processed according to [Test Developer name]’s Non-Conformance Reporting Requirements, and Medical Device Reports will be filed with the FDA as required. Through a process of inventory control, [Test Developer name] will also maintain records of device usage/purchase. [Test Developer name] will collect information on the performance of the test, and report to FDA any suspected occurrence of false positive or false negative results of which [Test Developer name] becomes aware. [Test Developer name] will maintain records associated with this EUA and ensure these records are maintained until notified by FDA. Such records will be made available to FDA for inspection upon request.
This section applies only to
the requirements of the Paperwork Reduction Act of 1995 The
burden time for this collection of information is estimated to
average 34 to 45 hours per response, including the time to review
instructions, search existing data sources, gather and maintain the
data needed and complete and review the collection of information.
Send comments regarding this burden estimate or any other aspect of
this information collection, including suggestions for reducing this
burden to the address to: Department
of Health and Human Services
An
agency may not conduct or sponsor, and a person is not required to Food
and Drug Administration
respond
to, a collection of information unless it displays a currently Office
of Operations
valid
OMB control number. Paperwork
Reduction Act (PRA) Staff DO
NOT SEND YOUR COMPLETED FORM TO THE PRA STAFF EMAIL ADDRESS
1 This template is part of the “Policy for Coronavirus Disease-2019 Tests During the Public Health Emergency (Revised),” available at https://www.fda.gov/regulatory-information/search-fda-guidance-documents/policy-coronavirus-disease-2019-tests-during-public-health-emergency-revised.
2 Available at https://www.fda.gov/regulatory-information/search-fda-guidance-documents/policy-coronavirus-disease-2019-tests-during-public-health-emergency-revised.
3 All EUA templates can be found at https://www.fda.gov/medical-devices/coronavirus-disease-2019-covid-19-emergency-use-authorizations-medical-devices/vitro-diagnostics-euas#covid19ivdTemplates.
4 Available at https://www.fda.gov/regulatory-information/search-fda-guidance-documents/emergency-use-authorization-medical-products-and-related-authorities.
5 Available at https://www.cdc.gov/csels/dls/sars-cov-2-livd-codes.html (last accessed on July 7, 2021). Note this website is not controlled by FDA.
6 Available at https://www.hhs.gov/coronavirus/testing/covid-19-diagnostic-data-reporting/index.html (last accessed on July 24, 2021). Note this website is not controlled by FDA.
7 Available at https://www.hhs.gov/sites/default/files/hhs-guidance-implementation.pdf (last accessed on July 24, 2021). Note this website is not controlled by FDA.
8 Available at https://www.hhs.gov/sites/default/files/non-lab-based-covid19-test-reporting.pdf (last accessed on July 24, 2021). Note this website is not controlled by FDA.
9 Available at https://www.fda.gov/medical-devices/postmarket-requirements-devices/quality-system-qs-regulationmedical-device-good-manufacturing-practices.
10 Further information regarding cybersecurity is available at https://www.fda.gov/medical-devices/digital-health/cybersecurity.
11 Available at https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-content-premarket-submissions-software-contained-medical-devices.
12 Available at https://www.fda.gov/regulatory-information/search-fda-guidance-documents/general-principles-software-validation.
13 Available at https://www.fda.gov/medical-devices/digital-health-center-excellence/device-software-functions-including-mobile-medical-applications.
14 Available at https://www.fda.gov/regulatory-information/search-fda-guidance-documents/shelf-software-use-medical-devices#:~:text=Off%2Dthe%2Dshelf%20(OTS,to%20run%20device%2Dspecific%20functions.
15 GISAID is a global science initiative and primary source that provides open-access to genomic data of influenza viruses and the novel coronavirus responsible for COVID-19. (See https://www.gisaid.org/ (last accessed on July 26, 2021). Note this website is not controlled by FDA.
16 For more information regarding evaluating the impact of viral mutations and variants, please see the guidance “Policy for Evaluating Impact of Viral Mutations on COVID-19 Tests” available at https://www.fda.gov/regulatory-information/search-fda-guidance-documents/policy-evaluating-impact-viral-mutations-covid-19-tests.
17 Available at https://www.fda.gov/medical-devices/coronavirus-covid-19-and-medical-devices/sars-cov-2-reference-panel-comparative-data.
18 Available at https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-informed-consent-vitro-diagnostic-device-studies-using-leftover-human-specimens-are-not.
19 Available at https://www.fda.gov/media/146695/download
20 All templates can be accessed at https://www.fda.gov/medical-devices/coronavirus-disease-2019-covid-19-emergency-use-authorizations-medical-devices/vitro-diagnostics-euas#covid19ivdTemplates.
21 Available at https://www.fda.gov/about-fda/cdrh-transparency/clia-waiver-application-decision-summaries.
22 Available at https://www.fda.gov/about-fda/cdrh-transparency/clia-waiver-application-decision-summarieshttps://www.cdc.gov/flu/dxfluviruspanel/index.htm (last accessed on September 22, 20209).July 2, 2021). Note this website is not controlled by FDA.
23 A list of EUA-authorized tests and their accompanying fact sheets are available at https://www.fda.gov/medical-devices/coronavirus-disease-2019-covid-19-emergency-use-authorizations-medical-devices/vitro-diagnostics-euas.
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| Author | McFarland, Scott |
| File Modified | 0000-00-00 |
| File Created | 2025-12-05 |
© 2026 OMB.report | Privacy Policy