Health Insurance Issuer Submission of the Preliminary Justification
Rate Increase Disclosure and Review Reporting Requirements (CMS-10379)
2024 PY URR instructions clean - 8-8-24
Health Insurance Issuer Submission of the Preliminary Justification
OMB: 0938-1141
OMB control number: 0938-1141
Expiration date: XX/XX/XXXX
 DEPARTMENT
OF HEALTH &
HUMAN
SERVICES
DEPARTMENT
OF HEALTH &
HUMAN
SERVICES
Centers for Medicare & Medicaid Services
Unified Rate Review Instructions

Rate
Filing
Justification:
Parts
I,
II,
and
III
Effective for Plan Years Starting on or after January 1, 2024
The contents of this document do not have the force and effect of law and are not meant to bind the public in any way, unless specifically incorporated into a contract. This document is intended only to provide clarity to the public regarding existing requirements under the law.
Contents
1.4 Market Reform Rating Rules 7
1.5 Guaranteed Renewability and Uniform Modification of Coverage 10
2. Part I: Unified Rate Review Template 12
2.1 Worksheet 1 – Market Experience 13
2.1.1 General Information Section 13
2.1.2 Section I: Experience Period Data 14
2.1.3 Section II: Projections 15
Section 2.2 Worksheet 2 – Plan Product Information 19
2.2.1 Section I: General Product and Plan Information 19
2.2.2 Section II: Experience Period and Current Plan Level Information 23
2.2.3 Section III: Plan Adjustment Factors 26
2.2.4 Section IV: Projected Plan Level Information 30
Section 2.3 Worksheet 3 – Rating Areas 32
3. Part II: Written Description Justifying the Rate Increase 32
4. Part III: Actuarial Memorandum and Certification Instructions 33
4.1 Redacted Actuarial Memorandum 34
4.2 General Information Section 34
4.4.1 Experience and Current Period Premium, Claims, and Enrollment 35
4.4.4 Plan Adjusted Index Rate 41
4.4.6 Consumer Adjusted Premium Rate Development 43
4.6 Plan Product Information 43
4.6.2 Membership Projections 43
4.6.3 Terminated Plans and Products 44
4.7 Miscellaneous Instructions 44
4.7.1 Effective Rate Review Information (Optional) 44
4.7.3 Actuarial Certification 44
5.1 HIOS Submission Statuses 46
1. Overview
Section 2794 of the Public Health Service Act (PHS Act) and the implementing regulations, 45 CFR Part 154, establish requirements for issuers offering non-grandfathered health insurance coverage in the small group and/or individual markets to submit rate filing information on rate increases to the Centers for Medicare & Medicaid Services (CMS). Rate Filing Justification submissions must provide sufficient information for state or federal regulators to review rate filings for compliance with 45 CFR 154.215, 154.225, 147.102, and 156.80.
A Rate Filing Justification (RFJ) for single risk pool plans1 consists of the following three parts:
Part I - Unified Rate Review Template (URRT): The URRT is required for all single risk pool plans in the individual, small group, and combined markets. This includes single risk pool plans that experience no rate changes, rate decreases, as well as new single risk pool plans. It is intended to capture information needed to monitor premium increases of health insurance coverage offered through and outside an Exchange and ensure compliance with the single risk pool methodology, including allowable market level Index Rate adjustments to reflect risk adjustment payments and charges, and other federal rating requirements.
Part II - Written Description Justifying the Rate Increase (Consumer Justification Narrative): Part II is required only for rate increases in single risk pool products that are subject to review (i.e., a plan within the product has a rate increase of 15% or greater). Part II is a consumer-friendly narrative that provides the justification for the rate increase, describes the relevant Part I data, the assumptions used to develop the rate increase, and an explanation of the most significant factors causing the rate increase.
Part III - Rating Filing Documentation (Actuarial Memorandum): Part III is required for any rate increase in a single risk pool plan. It is also required for any rate filing containing Qualified Health Plans (QHPs) or whenever a state requires it to be submitted. It is required for all plans in states that do not have an Effective Rate Review Program2 and for which CMS is responsible for reviewing the rate filing. Part III is a memorandum that includes the actuarial reasoning and assumptions, justifications, and methodologies that support the entries in the URRT.
For questions regarding submission of rate filings, please contact the rate review inbox at ratereview@cms.hhs.gov.
CMS will publicly post the Part II written description and the information contained in Parts I and III of the RFJ that do not constitute trade secrets or confidential commercial or financial information as defined in HHS’s Freedom of Information Act (FOIA) regulations.3 The information for all single risk pool coverage proposed rate changes (regardless of whether the increase is subject to review) and all final rate changes will be posted at https://ratereview.healthcare.gov/ and at http://www.cms.gov/CCIIO/Resources/Data-Resources/ratereview.html.
A state with an Effective Rate Review Program must post on the state’s website at least the information contained in Parts I, II, and III of the RFJ that CMS makes available on its website (or provide a link to CMS’s web address for such information) for proposed rate increases subject to review.4 That information must be posted on a uniform date no later than the date specified by the Secretary in guidance. The deadline for a state with an Effective Rate Review Program to post the same information on all final rate increases (not just those subject to review) is no later than the first day of the annual individual market annual open enrollment period for the applicable calendar year.5
Annual Submissions
All health insurance issuers offering single risk pool products in the individual, small group, and/or combined markets must submit the applicable parts of the RFJ via the Unified Rate Review (URR) module in HIOS.6 Issuers should check the Final Bulletin regarding the Timing of Submission and Posting of Rate Filing Justifications for the applicable Filing Year for Single Risk Pool Coverage to determine when annual rate filings must be submitted.7
Tip:
An
“Annual Submission” has an effective date of January 1.
“Quarterly Submissions” have an effective date of April
1, July 1, or October 1.
Quarterly Submissions
Tip:
When submitting quarterly rate changes in the small group market,
make sure you file early enough to allow for regulatory review in
time to submit new rates to the SHOP.
Quarterly rate changes must be submitted at least 105 days prior to the effective date of the rate change, or such earlier deadline as established by the state. Quarterly submissions must be finalized at least 45 days prior to the effective date. Issuers offering QHPs in a Federally-facilitated Small Business Health Options Program (SHOP) should also be mindful of the data correction windows when a new Rates Table Template must be submitted. Rate filings should be submitted to allow for sufficient time for the review to be completed prior to submitting the Rates Table Template in the Plan Management module of HIOS during the data correction window.
Index Rates
All issuers with single risk pool plans are required to establish an Index Rate for an effective date of January 1 of each year and file the Index Rate with the applicable regulatory authority. This is the annual submission described above and will be labeled as the annual filing in the URR module of HIOS, even if the filing includes scheduled quarterly small group trend increases. Subject to state requirements, small group issuers are allowed to file subsequent submissions that reset the Index Rate, the market level adjustments, or the plan level adjustments for the remaining quarters of the calendar year. These are the quarterly submissions described above. The Index Rate in the quarterly filings should only reflect remaining quarterly effective dates in the same calendar year (i.e., rates for groups with effective dates in the subsequent calendar year should not be included).
Dental Plans
Only embedded pediatric dental benefits within a medical plan should be reflected in the URRT. Further, in order for the dental costs to be included in the URRT, the dental costs must be spread across the entire single risk pool in accordance with the market rating rules in calculating the projected Index Rate. Stand-alone dental plans should never be reflected in the URRT.
Grandmothered Plans
Issuers of plans subject to the CMS non-enforcement policy8 (also known as grandmothered plans) must submit a Preliminary Justification for any filing which includes a rate increase of 10% or more into the HIOS Rate Review Justification (RRJ) Module, which generally consists of Part I – Rate Increase Summary Form, Part II – Written Explanation of the Rate Increase, and Part III – Rate Filing Documentation. In states that do not have an Effective Rate Review Program, issuers are encouraged to submit the Preliminary Justification at least 60 days in advance of implementation of any rate increase which is subject to review. Instructions for submitting these types of plans can be found at: https://www.cms.gov/CCIIO/Resources/Forms-Reports-and-Other-Resources/Downloads/HIOS-Rate-Review-Technical-Instructions-for-States-and-Health-Insurance-Issuers.pdf.
Optional Benefits
ALL benefits offered in a plan must be embedded in that plan. If an issuer wants to offer an “optional” benefit, there are two options:
The issuer can create a separate product with the required Essential Health Benefits (EHBs) and the “optional” benefit included.
The issuer can offer the “optional” benefit as a separate policy in a manner that satisfies the definition of one of the categories of excepted benefits.9
The concept of “optional riders” is incongruent with federal rules, including the single risk pool requirements.
Issuers must comply with the Market Reform Rating Rules specified in 45 CFR 156.80 and 147.102. The following is a description of allowable rating methods and factors issuers may use when establishing their rates.
Single Risk Pool
The single risk pool, as specified in 45 CFR 156.80(a-c), includes ALL non-grandfathered covered persons (lives) an issuer has in a state, within a market (individual, small group, or combined). This includes information for transitional products/plans. However, for reporting purposes and build-up of the projected Index Rate, an issuer should only list transitional plan experience that actually affects the projected Index Rate. In other words, an issuer is not required to include transitional plan experience from the Experience Period, only to back that experience out when calculating the projected Index Rate. The Projection Period should reflect experience of transitional policies to the extent the issuer anticipates the members of those policies will be enrolled in single risk pool plans during the Projection Period.
Index Rate
Tip:
The Index Rate is the allowed claims PMPM for providing EHBs during
the applicable period.
If an issuer projects members in transitional policies to migrate to a single risk pool policy, appropriate adjustments should be made in Worksheet 1 – Section II of the URRT to bring the costs associated with the transitional policies in line with projected costs of the single risk pool policy in the projected experience. Projected member experience should reflect when those members are expected to enter a single risk pool plan. For example, transitional plan members expected to enroll in a single risk pool plan in October would contribute three months of projected experience.
Market-Wide Adjusted Index Rate
The Market-Wide Adjusted Index Rate (MAIR) is the Index Rate adjusted for payments and charges under the risk adjustment program and Exchange Fees (with impacts and costs spread across the whole risk pool). As a result, the MAIR should be the same value for ALL non-grandfathered plans for an issuer in a state and market.
Plan Adjusted Index Rate
The Plan Adjusted Index Rate (PAIR) is the MAIR Rate further adjusted for ONLY the plan specific factors allowed by 45 CFR 156.80(d)(2), which are:
Actuarial value and cost-sharing design of the plan.
The plan’s provider network, delivery system characteristics, and utilization management practices.
Benefits provided under the plan that are in addition to EHBs.
Administrative costs, excluding Exchange user fees (which are already accounted for in the MAIR).
Only catastrophic plans may be adjusted for the expected impact of the special eligibility categories of these plans. If an adjustment is made to catastrophic plans, this adjustment may not be recovered elsewhere in the rating process, as that would be seen as removing the catastrophic plan experience from the single risk pool.
Tip:
The only allowable plan adjustments are found in 45 CFR
156.80(d)(2). “Other” is not an allowable plan
adjustment.
Calibration
The PAIR must be calibrated for plans within the single risk pool to correspond to an age rating factor of 1.0, a geographic rating factor of 1.0, and a tobacco use rating factor of 1.0.10 The intent of the calibration factors is to reset the PAIR so that applying the age factor, geographic rating area factor, and tobacco use factor will result in the appropriate consumer adjusted premium rate for an individual age X, living in rating area Y, with the applicable tobacco load factor applied.
For each of the allowable rating factors of age, geography, and tobacco use; there is ONLY ONE calibration allowed. That is, the calibration from the single risk pool to the allowable rating factors may not vary by plan; it must be a common adjustment for all plans in a state and market. The ONLY allowable consumer level premium rate modifiers that can be calibrated are age, geography, and tobacco use.
It is important to note that the calibration process should ONLY occur after the PAIR has been determined, not at any point before. The cost of all benefits (EHB and non-EHB) and other expenses may not be charged to the consumer using a flat dollar amount. All components under the plan must be part of the premium charged. All components of the premium are subject to the consumer level rating adjustments, and therefore, all components of the premium should likewise have the calibration applied to them.
Fees
Fees and costs are included in the premium and applied at the plan level as part of the distribution and administrative costs adjustment. The only exception is the application of the Exchange user fees, which are applied to the Index Rate at the market level as instructed by 45 CFR 156.80(d). All other fees must be included in the development of the PAIR, prior to the application of member level rating factors, such as age factors. No additional fees may be charged outside of the development of the PAIR. For example, if it costs an issuer $35 to process an application, that cost must be included in the premium rate development of all policies (new issues and renewals) and subject to the member level rating factors such as age, geographic rating, and tobacco use factors. The issuer may not, in that example, charge a $35 fee per policy for submission of the application.
Consumer Adjusted Premium Rate
The Consumer Adjusted Premium Rate is the final premium rate for a plan that is charged to an individual, family, or small employer group after applying the rating and premium adjustments in the applicable Market Reform Rating Rules. The Consumer Adjusted Premium Rate is developed by calibrating the PAIR to the age curve as described above, calibrating for geography and tobacco use if necessary, and applying the allowable rating factors.11 Allowable rating factors, found in 45 CFR 147.102(a), are as follows:
Family Structure: Family structure takes into account family composition and the maximum of three under-age-21 child dependents. The total premium for family coverage is determined by summing the premiums for each individual family. With respect to family members under the age of 21, the premiums for no more than the three oldest covered children must be taken into account in determining the total family premium. This adjustment does not result in a separate rating factor. Family tiering only occurs in states that use pure community rating and is uniformly applied to all plans in the risk pool (tier information available at: https://www.cms.gov/CCIIO/Programs-and-Initiatives/Health-Insurance-Market-Reforms/state-rating#family).
Rating Area: Geographic rating areas are specific to each state, and all issuers in the state are required to follow them. Issuers may only set one rating factor per rating area, per state, per market, and that factor must apply uniformly to all plans the issuer has in that rating area. If an issuer has multiple networks within a given rating area and wants to develop premiums specific for each network, the issuer must have a separate plan for each network in the rating area. Geographic factors should only reflect differences in the cost of delivery (which can include both unit cost and provider practice pattern differences). Geographic factors may not reflect differences in morbidity by region. State specific geographic rating areas are available at: https://www.cms.gov/CCIIO/Programs-and-Initiatives/Health-Insurance-Market-Reforms/state-gra.
Age Factor: Once the PAIR is calibrated to a 1.0 value on the age curve, the entire set of age rates is determined using the standard age factor of each age. The age factors must be the standard age curve set by HHS or a state specific age curve (if the state requires different age factors than the standard federal age curve).12
Tobacco Use: A tobacco use surcharge (limited to 50% of the Consumer Adjusted Premium Rate) may be applied to individuals who may legally use tobacco under federal and state law.
The following graphic depicts the flow of the Index Rate development process:
 Figure
1 Flow of the Index Rate
development process
Figure
1 Flow of the Index Rate
development process
Issuers should review 45 CFR 147.106(e), 146.152(d) and (f), 148.122(e), and 144.103 when determining if a product or plan is considered to be the same product or plan for rate review purposes. Note that changing the HIOS Product or Plan ID does not necessarily result in the product or plan being considered new for rate review purposes.
In the individual, small group, and combined markets, product modifications made uniformly at the time of coverage renewal and solely pursuant to applicable federal or state requirements are considered a uniform modification of coverage if the modification is made within a reasonable time period after the imposition or modification of a federal or state requirement, and the modification is directly related to the imposition or modification of the federal or state requirement. For example, if the federal or state government mandates coverage of a new benefit, existing products may be altered to include coverage of the mandated benefit without being considered “new” products.
A modification made uniformly at the time of coverage renewal in the individual, small group, or combined market is also considered to be a uniform modification of coverage if the resulting health insurance coverage for the product meets the following criteria:
The product is offered by the same health insurance issuer or a member of the issuer’s controlled group.
The product network type remains the same, for example a health maintenance organization remains a health maintenance organization, or a preferred provider organization remains a preferred provider organization.
The product continues to cover a majority of the same service area.
Within the product, each plan has the same cost-sharing structure as before the modification, except for any variation in cost sharing solely related to changes in cost and utilization of medical care, or to maintain the same metal tier level.
The product provides the same covered benefits (i.e., covered items and services), except for changes in benefits that cumulatively impact the PAIR for any plan within the product within an allowable variation of ±2 percentage points (not including changes pursuant to applicable federal or state requirements).
A state may broaden the standards mentioned in the third and fourth bullet points, so an issuer may need to check with the state to determine if a change to a product’s service area or cost-sharing structure is considered to be a uniform modification of coverage.
In addition, an issuer is not considered to have discontinued offering all health insurance coverage in a market if the issuer or a member of the issuer’s controlled group continues to offer and make available for enrollment in the applicable market in the state at least one product of the original issuer that is considered to be the same product, meaning that any change to the product is within the scope of uniform modification. For this purpose, ‘‘controlled group’’ means a group of two or more persons that is treated as a single employer under sections 52(a), 52(b), 414(m), or 414(o) of the Internal Revenue Code, 26 U.S.C. 1, et seq.
States that interpret or apply market withdrawal provisions differently under state law are not prohibited from considering the transfer of all products in a market to a different issuer within a controlled group to be new products and the scenario a market withdrawal. A controlled group may be defined more narrowly under state law—that is, a controlled group may be defined to not include all of the entities that would be included under the federal definition.
Issuers that replace an entire portfolio of products in a market with new products may also avoid a 5-year ban under the market withdrawal provision provided the issuer reasonably identifies which newly offered product (or products) is replacing the discontinued product (or products) and subjects the new product (or products) to the federal rate review process, where the process is otherwise applicable to the type of product and market. An issuer’s identification of which new product replaces which discontinued product will be considered reasonable if it reflects the issuer’s expectations regarding significant transfer of enrollment from one product to the other (for example, because the products have been cross-walked for that purpose). Issuers should identify which new product replaces which discontinued product in the actuarial memorandum. This provides a way for issuers to completely revise their product portfolio offerings without triggering a 5-year ban, provided they are not revising all of their products simply to avoid rate review. Issuers that do not adhere to these conditions will be considered to have effectuated a market withdrawal subject to the 5-year ban on market re-entry.
2. Part I: Unified Rate Review Template
The Unified Rate Review Template (URRT) is intended to help regulators review rates for single risk pool plans for compliance with the Affordable Care Act and determine whether proposed rate increases subject to review are unreasonable. The URRT also collects data from issuers so that CMS can fulfill its duty to monitor premium increases inside and outside of the Exchanges. This includes single risk pool plans that experience no rate changes, rate decreases, as well as rates for new single risk pool plans. The ‘Submission Level Rate Increase %’ and ‘Product Rate Increase %’ on Worksheet 2 of the URRT will display on the CMS website, regardless of the size of the change. If a plan within a product has a rate increase of 15 percent or greater (i.e., the product is subject to review), HIOS will require the issuer to enter a written description justifying the product rate increase. The written justification will also be displayed on the CMS website.
It is critically important that issuers provide accurate and complete information in the URRT. Failure to provide accurate information in the first submission increases the likelihood that state or federal regulators will need to request additional information. Issuers must respond promptly to all questions from the applicable regulator(s). Failure to provide information on a timely basis or failure to provide accurate information slows the review process and puts issuers at risk for missing critical deadlines to offer products and plans in the individual, small group, and combined markets. Issuers should verify that the data entered in the URRT is consistent with decimal place limits and instructions to avoid delays in the review process. Issuers should not finalize a URRT containing input cells with formula links, as this can cause problems with the file once it has been uploaded into HIOS. If formula links are used to bring input data into the URRT, be sure to copy and paste values in the input cells before clicking “Finalize” in the template.
Tip:
If copying and pasting values into the URRT, make sure pasted values
are consistent with decimal place limits and formatting instructions
found within the URRT cells. Do not finalize a URRT that has linked
formulas in the input cells.
2.1 Worksheet 1 – Market Experience
The purpose of Worksheet 1 of the URRT is to capture information at the market level for non- grandfathered individual and small group (or combined) products, consistent with the requirement to set premium rates using a single risk pool, as defined in 45 CFR 156.80. The worksheet is not intended to prescribe a rate development methodology. Rather, the worksheet captures Experience Period data and key assumptions consistent with those used in the development of the MAIR. There are three sections in this worksheet.
General Information Section: Captures information about the issuer, state, and the health insurance market to which the proposed rate changes will apply.13 This information is displayed on Worksheets 1 and 2 of the URRT.
Section I (Experience Period Data): Captures summarized historical financial and enrollment information from a recent historical Experience Period.
Section II (Projections): Captures projections for factors such as trend, demographics, changes in plan design, and other information for the upcoming plan year.
Company Legal Name: Enter the organization’s legal entity name. The name entered in this cell must be the name that is associated with the HIOS Issuer ID.
State: Enter the state that has regulatory authority over the policies. A separate template must be completed for each state in which the issuer is offering single risk pool products in the individual or small group (or combined) market.
HIOS Issuer ID: Enter the HIOS ID assigned to the legal entity.
Market: Select the applicable market from the drop-down box. Valid markets are Individual, Small Group, or Combined.
The market chosen must be consistent with the state’s determination of their allowable markets (i.e., if a state requires issuers to merge the individual and small group markets into a single risk pool with the same plan options, the issuer must choose “Combined”).
Effective Date of Rate Change(s): This is the effective date for which rates are being submitted. This field is automatically populated based on the latest “Effective Date of Proposed Rates” entered in Row 19 of Worksheet 2. All new and renewing products and plans must have the same effective date.
If the submission is for the individual or combined markets, the effective date must be January 1 of the year for which rates are being submitted. If the submission is for the small group market, enter the effective date for which the Index Rate is being revised. For example, if the small group submission revises the Index Rate for July 1, 2021 and includes a trend increase applicable on October 1, 2021, enter July 1, 2021 as the effective date.
The financial and enrollment information entered in this section should reflect the experience of all non- grandfathered policies used in building up the rates for the specified market and state. The information is intended to reflect the single risk pool for the market as required by 45 CFR 156.80. The information in this section should reflect historical financial and enrollment information for the identified legal entity only, except in cases where legal entities combine to provide coverage as a “joint” policy. A “joint” policy in this case refers to an arrangement between licensed entities where each entity covers a part of the total benefits (e.g., a Point of Service type plan where an HMO entity offers in-network benefits, while a licensed insurance company offers out-of-network benefits). In order to be considered a “joint” policy, the coverage from both licensed entities must be purchased together, and the “joint” policy cannot be offered as stand-alone coverage.
Experience Period: Enter the first date of the Experience Period.
The Experience Period must be a twelve-month period. The template calculates the end date of the Experience Period such that the period is twelve months long.
For individual and combined market submissions, the Experience Period must be a calendar year period. It should be the most recently completed calendar year. Therefore, the first date of the Experience Period must be January 1. For small group market submissions, the first date of the Experience Period must be the first date of a calendar quarter (i.e., January 1, April 1, July 1, or October 1).
The Experience Period reflects a period during which premiums were earned and claims were incurred. For example, if the Experience Period is January 1, 2021 through December 31, 2021, the issuer may include claims payments through a date beyond the end of the Experience Period (e.g., February 28, 2022) for claims with dates of service within the Experience Period when estimating the total claims incurred during the period. The paid through date is not captured in the template, but is requested in the Actuarial Memorandum.
Allowed Claims: Enter total allowed claims with dates of service during the Experience Period.
Allowed Claims are defined as the total payments made under the policy to healthcare providers on behalf of covered members and include payments made by the issuer, member cost-sharing, cost-sharing paid by HHS on behalf of low-income members, as well as net payments from any federal or state reinsurance arrangement or program. Consequently, allowed claims should include actual payments made and estimates of claims incurred but not reported during the period. See the Actuarial Memorandum instructions for guidance related to incurred but not reported claim reserve documentation. Allowed Claims also include claims not tied to a specific date of service, such as capitation or risk sharing payments, if the payments were for services provided during the Experience Period. They include claims for EHBs as well as non-EHBs. This would not include the amount of billed charges the member must pay in excess of the issuer’s contractual allowed amount (often described as “balance billing”).
By definition, “Allowed Claims” do not include:
Ineligible claims, such as duplicate claims, third party liabilities (e.g., coordination of benefits claims), and any other claims that are denied under the policy terms.
Payments for services other than medical care provided, (e.g., medical management, quality improvement, and fraud detection and recovery expenses) even if these amounts are included in claims for Medical Loss Ratio (MLR) reporting purposes.
Active life reserves (policy reserves, contract reserves, contingency reserves, or any kind of reserves except traditionally defined reserves for claims incurred but not reported) or change in such reserves.
Charges or payments from the federal risk adjustment program.
Reinsurance: Enter any claims reimbursement received through a federal or state reinsurance program, net of any reinsurance fees.
Incurred Claims in Experience Period: Enter total claims incurred in the Experience Period.
Incurred claims are defined as Allowed Claims (defined above) less member cost-sharing, cost-sharing paid by HHS on behalf of low-income members, as well as any net payments from a federal or state reinsurance arrangement. Incurred claims includes claims for EHBs and non-EHBs.
Member cost-sharing is defined as payments made against the Allowed Claims by the member for health care services (e.g., deductible, coinsurance, and copayments). This does not include premium or the amount of billed charges the member must pay in excess of the issuer’s contractual allowed amount (often described as “balance billing”).
Risk Adjustment: Enter the transfer payments or charges from the federal risk adjustment program.
Transfer amounts should include the high cost risk pool adjustment to claims and any assessment to pay for those claims. The risk adjustment user fee should not be included here, but rather in the taxes and fees portion of administrative costs. Payments made to an issuer from the risk adjustment program should be entered as a positive amount, while charges assessed to an issuer should be entered as a negative amount.
Risk adjustment should account for Risk Adjustment Data Validation (RADV) adjustments, including default data validation charges (DDVCs) and allocations, as appropriate.
In some cases the risk adjustment payment or charge from the Experience Period may not be final. Issuers should provide their best estimate in these cases.
Experience Period Premium: Enter the amount of premium earned during the Experience Period.
This should simply be the premium earned and should not reflect any MLR rebates
Experience Period Member Months: This number is automatically calculated from Worksheet 2 and should reflect the total number of member months from the Experience Period.
The section begins with the Index Rate of the Experience Period, broken out by benefit category, and applies trend and other adjustments to arrive at the MAIR. The information entered here should represent the actuary’s best estimate.
2.1.3.1 Benefit Category and Manual Rate
Several fields listed below require issuers to enter data by Benefit Category. The preferred definitions for each Benefit Category follow:
Inpatient Hospital: Includes non-capitated facility services for medical, surgical, maternity, mental health and substance abuse disorder, skilled nursing, and other services provided in an inpatient facility setting and billed by the facility.
Outpatient Hospital: Includes non-capitated facility services for surgery, emergency services, lab, radiology, therapy, observation, and other services provided in an outpatient facility setting and billed by the facility.
Professional: Includes non-capitated primary care, specialist, therapy, the professional component of laboratory and radiology, and other professional services, other than hospital based professionals whose payments are included in facility fees.
Other Medical: Includes non-capitated ambulance, home health care, DME, prosthetics, supplies, vision exams, dental services, and other services.
Capitation: Includes all services provided under one or more capitated arrangements.
Prescription Drug: Includes drugs dispensed by a pharmacy. This amount should be net of rebates received from drug manufacturers.
Experience Period Index Rate PMPM: The Index Rate from the Experience Period should be broken out by the benefit categories listed above.
The Index Rate is the average allowed claims PMPM for providing EHBs within the single risk pool of the state market. It is the legal entity-specific rate for the market that is being submitted (i.e., the issuer’s individual, small group, or combined market). It is the Allowed Claims PMPM for EHBs only.
Year 1 and Year 2 Trend: The Experience Period Index Rate should be trended forward to the Projection Period by benefit category. The trend should be broken out between cost and utilization.
The Experience Period Index Rate is multiplied by the cost and utilization trend factors for years 1 and 2. Trend should be entered as one plus the trend amount (e.g., a 3.5% cost trend for Year 1 should be entered as 1.035). For quarterly small group filings, the terms “Year 1” and “Year 2” are used loosely. Depending upon the Experience Period and Projection Period used, Years 1 and 2 might not cover a 12 month period. The trend rates entered should be the applicable trend that takes the Experience Period Index Rate to the MAIR for the effective date of the filing. For example, if an issuer were to file a third quarter rate increase, the trends entered should lead to a projected Index Rate and MAIR for July 1. Once the permitted plan-level adjustments and calibrations are applied, the Calibrated Plan Adjustment Index Rate should be the effective base rate for July 1. Applying the appropriate age, rating area, and tobacco use factors should generate consumer premium rates effective July 1. The trend calculation should be explained in the actuarial memorandum.
Trended EHB Allowed Claims PMPM: This is automatically calculated in the spreadsheet by applying Years 1 and 2 cost and utilization trends to the Experience Period Index Rate PMPM.
2.1.3.2 Adjustments to EHB Allowed Claims PMPM
Morbidity Adjustment: Enter the assumed change in morbidity of the covered population from the Experience Period to the Projection Period.
“Change in morbidity” means that component of the change in average allowed claims PMPM that will occur under the circumstances where all demographic (e.g., age, gender, and region) and product mix, and all provider network contracts and time parameters (i.e., trends = 0) are held constant on the population that exists in the Experience Period.
The change in morbidity must be entered as 1 plus the total anticipated percent change in morbidity from the Experience Period to the Projection Period. For example, if in a 24-month period from the Experience Period to the Projection Period the morbidity is expected to increase by 10%, enter 1.100. Similarly, if the morbidity is expected to decrease by 10% over the 24- month period, enter 0.900.
Some of the adjustments issuers might include are:
Take-up rate of the uninsured (the percent of currently uninsured that purchase coverage during the Projection Period)
Health status of newly insured
Induced demand of newly insured
Pent-up demand of newly insured
Subsidy effects
A description of the methodology used to develop the adjustment must be included in the actuarial memorandum.
Demographic Shift: Enter the assumed change in allowed claims due to demographic shifts of the covered population from the Experience Period to the Projection Period. Demographics may include things like age, gender, and geographic area changes in the population.
Similar to the morbidity adjustment, the change in demographics should be entered as 1 plus the total anticipated percent change in allowed claims related to demographic changes from the Experience Period to the Projection Period.
The methodology used to develop the adjustment must be included in the actuarial memorandum.
Plan Design Changes: Enter the assumed change in EHB allowed claims due to plan design changes.
The change should be entered as 1 plus the total anticipated percent change in EHB allowed claims. For example, if plan design changes are expected to decrease allowed EHB claims by 3.5%, enter 0.965 in the field.
Other: Enter the assumed change in cost related to things other than a change in Morbidity, Demographic Shift, or Plan Design Changes.
The “Other” change must be entered as 1 plus the total anticipated percent change in EHB allowed claims from the Experience Period to the Projection Period.
Some of the adjustments an issuer might include in this section are:
Legislative changes affecting the market.
Changes brought about by State Relief and Empowerment Waivers under section 1332 of the Affordable Care Act.
A description of what is included in the adjustment and the methodology used to develop the adjustment must be included in the Actuarial Memorandum.
Adjusted Trended EHB Allowed Claims PMPM for MM/DD/YYYY: This is automatically calculated in the spreadsheet by applying the morbidity adjustment, demographic shift, plan design changes, and other adjustments to the Total Trended EHB Allowed Claims PMPM.
Manual EHB Allowed Claims PMPM: In cases where the issuer’s experience is not credible, a manual rate for EHB allowed claims can be entered here. An explanation of how the manual rate was developed should be included in the actuarial memorandum if an issuer uses a manual rate.
Applied Credibility %: Enter the credibility percentage that should be applied to the Trended EHB Allowed Claims PMPM. For fully credible experience, enter 100% in this field.
2.1.3.3 Adjustments to the Projected Index Rate
Projected Index Rate for MM/DD/YYYY: This field is automatically calculated in the URRT by weighting the Adjusted Trended EHB Allowed Claims PMPM and Manual EHB Allowed Claims PMPM by the Applied Credibility % entered above.
This should be the projected Index Rate, which is the Allowed Claims PMPM for EHBs only.
Reinsurance: Enter any expected net reinsurance recoverables received through a state or federal reinsurance program here on an allowed amount PMPM basis. Since the Projected Index Rate represents EHB allowed claims, the reinsurance amount entered here should be grossed up by the paid to allowed average factor.
While state reinsurance payments are not identified as an allowable adjustment to the Index Rate in 45 CFR 156.80, this is an appropriate place to enter reinsurance amounts for reporting purposes. Amounts an issuer receives as reinsurance payments should be entered as a positive number. For example, if an issuer expects to receive $10.75 PMPM in net reinsurance payments on an allowed basis, then $10.75 should be entered in this field.
Risk Adjustment Payment/Charge: Enter the projected PMPM amount of risk adjustment transfers for the Projection Period. The value should reflect the actual PMPM amounts expected in the Projection Period. However, the net risk adjustment transfer amount applied in the calculation of the MAIR should be grossed up by the paid-to-allowed average factor as the Index Rate and MAIR reflect claim costs on an allowed basis.
Transfer amounts should include the high cost risk pool adjustment to claims and any assessment to pay for those claims. The risk adjustment user fee should not be included here, but rather in the taxes and fees portion of administrative costs. If the issuer expects to receive a projected risk adjustment payment, then the entry should be a positive value. If the issuer expects to owe a projected risk adjustment charge, then the entry should be a negative value.
As previously mentioned, risk adjustment should account for RADV adjustments, including DDVCs and allocations, as appropriate.
The calculation of the projected risk adjustments should consider the appropriate published transfer equation. Please describe the methodology for estimating the PMPM amount in the Actuarial Memorandum.
Exchange User Fees: Enter the expected exchange user fees as a percentage charge.
Remember we are dealing with claims on an allowed basis at this point. A description of the process the issuer used to calculate the adjustment should be provided, along with a narrative that demonstrates that the Exchange user fees are applied as an adjustment to the Index Rate at the market level. The value should reflect the expected mix of Exchange and non-Exchange enrollees.
Market Adjusted Index Rate: The template calculates a MAIR by subtracting the amounts entered for reinsurance and risk adjustment (so a negative risk adjustment entry results in an increase to the MAIR) and dividing by 1 minus the exchange user fee percentage.
The MAIR calculation flows into Worksheet 2 where the allowable plan adjustment factors are applied to determine the PAIR. For annual filings, this should be the Index Rate that applies for the first quarter. For quarterly small group filings, the Index Rate should represent the Index Rate applicable to the initial quarter being changed. For instance, a small group rate filing applicable to the third and fourth quarter rates should reflect the third quarter Index Rate.
Projected Member Months: This field is automatically pulled from Worksheet 2.
Section 2.2 Worksheet 2 – Plan Product Information
The purpose of Worksheet 2 is to capture information at the product and plan level. The worksheet captures information on Experience Period data, Plan Adjustment Factors, Projection Period data, and other information related to each product or plan. There are four sections in this worksheet.
Section I (General Product and Plan Information) captures information about each product and plan. This includes general information such as the plan and product IDs, along with more specific information such as the effective date, Actuarial Value (AV), and rate change.
Section II (Experience Period and Current Plan Level Information) captures current and historical information such as premium and claims in a more detailed manner than in Worksheet 1. Information related to risk adjustment transfer charges and payments, reinsurance, and current membership is also collected.
Section III (Plan Adjustment Factors) collects the allowable plan level adjustments found in 45 CFR 156.80(d)(2) and the calibration factors discussed in 45 CFR 156.80(d)(3).
Section IV (Projected Plan Level Information) captures similar information collected in Section II, for the Projection Period.
2.2.1 Section I: General Product and Plan Information
All products and plans included in the single risk pool must be accounted for on Worksheet 2 of the URRT. Each non-transitional plan that will be offered for sale must have its own column in the URRT indicating if the plan is new or renewing, along with an appropriate rate change entered in the Cumulative Rate Change % (over 12 months prior) field (Field 1.11) of the URRT. Each plan offered in the experience period, but terminated prior to the effective date of the filing, should also have its own column indicating the plan will be terminated. Transitional plan experience included in Worksheet 2 may be combined and entered under a single plan.
Terminated plans should have Experience Period information entered in Section II of the URRT, but Sections III and IV will be populated with 0. If members in a plan being terminated are mapped into a new or renewing plan(s), the projected experience of those members being mapped should be reflected under the mapped plan(s) in Section IV.
Product Name: Enter the product name in the corresponding column(s).
The term “product” means a discrete package of health insurance benefits a health insurance issuer offers using a particular product network type (e.g., HMO, PPO, EPO, POS, etc.) within a service area. “Product” has the same meaning as included in 45 CFR 154.102 and 144.103.
Tip:
HIOS does not report product or plan names containing special
characters. Consider spelling out name of special characters (e.g.,
“20Percent Coinsurance” rather than “20%
Coinsurance”).
Product ID: Enter the product ID that corresponds with each product. The two-letter state code portion of the Product ID must be entered using capital letters.
The “Product ID” should be the product number assigned by HIOS. Each product included in the single risk pool must be identified in Worksheet 2 of the template.
Plan Name: Enter the name of each plan within a product.
The term “plan” means, with respect to an issuer and a product, the pairing of the health insurance coverage benefits under the product with a particular cost-sharing structure, provider network, and service area. Most products will consist of multiple plans where each plan must have an AV equal to one of the permitted metal levels or catastrophic coverage, and most products will have multiple metal levels represented under a single product. The Plan Name is the marketing name used when referring to the specific set of benefits and cost-sharing values. The Plan Name shown should be consistent across submissions (e.g., QHP application, state filings). All plans included in the single risk pool must be entered in this section of Worksheet 2. This includes any plans that are terminated but have experience included in the single risk pool during the Experience Period. It also includes any plans that were not in effect during the Experience Period but were made available thereafter. Issuers should not enter cost-sharing reduction plan variations separately, since as described in 45 CFR 156.400 through 156.420, plan variations are not separate plans, but rather variations of the corresponding standard plans with the same premium, benefits, and network as the standard plan.
Currently, HIOS does not report plan names containing special characters (e.g., “%”). It is recommended that plans containing special characters spell out the name of the special character (e.g., “20 Percent Coinsurance Plan” should be entered instead of “20% Coinsurance Plan”).
Plan ID (Standard Component ID): Enter each assigned Plan ID. The two-letter state code portion of the Plan ID must be entered using capital letters.
The Plan ID is a unique identifier for the set of benefits and cost-sharing values offered within a product by the HIOS issuer, or in other words, a unique identifier of each plan. Plan IDs include multiple digits. The first ten digits are the Product ID, and the next four identify the unique plan within the product. This field must be entered as a text input and must include any leading zeroes (e.g., 0030).
Generally, if a plan is the “same plan” as the previous year, it should maintain the same HIOS Standard Component (plan) ID. There are exceptions to this, such as if a plan were to change metal tiers from one plan year to the next. Even though this plan may be defined as the same plan under 45 CFR 144.103, risk adjustment reporting requires this plan to receive a new Plan ID. Note that in this situation an issuer should still identify the plan as “renewing” even though it has a new Plan ID.
Metal: For each plan within a product, choose the corresponding metal level from the drop down menu in the template. Plans that are included in a QHP certification application must show the same Metal as is shown in the QHP application.
A “Not Applicable” selection should be made when the AV metal level does not apply to a plan such as a non-single risk pool plan.
The ACA requires that non-grandfathered plans offered in the individual or small group (or combined) market must have an AV that corresponds to a defined metal level. The metal AVs are defined in 45 CFR 156.20 as “the percentage paid by a health plan of the percentage of the total allowed costs of benefits.” There are five levels of coverage that can be offered: Platinum, Gold, Silver, Bronze, and Catastrophic. The AVs for each of these metal levels are shown in the table below. The AV used in determining the metal level must be based on the AV Calculator or an acceptable alternative if a health plan’s design is not compatible with the AV Calculator.
The AV used to determine the metal level must be within a de minimis variation from the AVs defined in the ACA.
Table 1 Metal Level
-
Metal Level
AV Requirements
Platinum
90%
Gold
80%
Silver
70%
Bronze
60%
Catastrophic
Not specified by law*
*Catastrophic level – a plan offered in the individual market only that is only available to individuals who are below the age of 30 before the beginning of the plan year or who have received a certificate of exemption based on affordability or hardship.
For single risk pool plans that are terminated prior to the Projection Period, enter the metal level of the plan just prior to termination.
The “Not Applicable” selection should be made in the case of non-single risk pool products or plans that are reported in the Experience Period.
AV Metal Value: For each plan, enter the corresponding AV value that results from the AV Calculator or a permissible alternative method that complies with 45 CFR 156.135(b).
For non-single risk pool products that are reported in the Experience Period, enter zero.
For single risk pool plans that are terminated prior to the Projection Period, enter the prior metal AV value for the plans.
For catastrophic plans, enter an approximate AV Metal Value for the plan (e.g., 0.580). Since there is not a catastrophic continuance table within the AV Calculator, actuaries should use their best judgment in estimating the AV Metal Value.
Plan Category: Use the dropdown box to identify plans as New, Renewing, or Terminated.
Remember a selection of “Renewing” for a plan with a 15% or greater annual increase will result in HIOS identifying the product as subject to review and will require the issuer to enter a Consumer Justification Narrative for that product.
An existing issuer must have at least one “Renewing” plan, otherwise the issuer may be considered to have exited the market. Revisit Section 1.6 above for more information.
Plan Type: Select the applicable plan type from the drop-down box. Valid Plan Types are Indemnity, PPO, POS, HMO or EPO.
In the event that the list of plan types does not describe an issuer’s plan exactly, the issuer should select the closest plan available and provide further explanation of the Plan Type in the Actuarial Memorandum.
Tip:
A Product should have only one Plan Type listed under it. A single
product may not contain both HMO and PPO network types.
Exchange Plan?: For each plan, select an indicator (Yes or No) from the drop-down box as to whether the plan will be offered inside a State-based Exchange (SBE), Federally-facilitated Exchange (FFE), or Small Business Health Options Program (SHOP), regardless of whether or not it will also be offered or marketed outside the Exchange. If an application for QHP status is pending, enter “Yes.” This indicator should not be used to identify whether a plan is offered on a private Exchange. If you indicate “Yes” for a plan offering full EHB, the plan will automatically be considered as available on and off the Exchange, due to guaranteed availability. Exchange issuers are required to make all full EHB plans available upon request from consumers who meet the guaranteed availability and EHB requirements, but are not required to market or actively sell Exchange plans outside the Exchange.
For terminated plans, the issuer should enter “No” in this field, even if the plan was offered on the Exchange just prior to its termination.
Effective Date of Proposed Rates: For each plan, enter the corresponding effective date of the proposed rates.
All non-terminating products and plans must have the same effective date.
If the submission is for the small group market, enter the effective date on which the products’ rates will change due to the Index Rate being revised. For example, if the small group quarterly submission revises the Index Rate for a July 1, 2020 effective date and includes a trend increase applicable on October 1, 2020, enter July 1, 2020.
Cumulative Rate Change % (over 12 months prior): Enter the average change in premium rates over the twelve month period prior to the effective date for each plan. This should be the premium- weighted average of the 12-month changes that apply at renewal.
This should be measured as the change in premium rates tables over the 12 month prior rate table using the plan’s current distribution of enrollment by age, geographic area, and tobacco status. For small group quarterly rate filings, this should reflect the weighted rate change across all remaining quarters in the year.
This is the rate change that determines whether the renewing product is subject to review, per 45 CFR 154.200. This field is also the HIOS trigger to identify a rate increase subject to review. If any renewing plan within a product has a rate increase of 15% or greater, HIOS will require submission of Part II, the written description justifying the rate increase for that product.
Issuers should enter 0% in this field for terminating plans.
Product Rate Increase %: The template calculates the average rate increase for each product by weighting the Cumulative Rate Change Percent (over 12 months prior) for each renewing plan within the product using Current Enrollment and the Current Premium PMPM.
Tip:
Make sure information entered into the URRT is correct. Information
submitted in the URRT will determine the requested rate increase
shown on the CMS website.
Submission Level Rate Increase %: The template calculates the submission level rate increase by weighting each renewing plan within the submission using Current Enrollment and the Current Premium PMPM.
Similar to the Product Rate Increase % above, if a plan is identified as New or Terminated in the Plan Category field or has a Metal designation of “Not Applicable,” that plan’s Cumulative Rate Change will not be counted toward the Submission Level Rate Increase Percent.
This is the submission level rate increase that will appear when proposed and final rate changes (regardless of whether the increase is subject to review) are released at https://ratereview.healthcare.gov/. Rate changes of zero will not be posted.
2.2.2 Section II: Experience Period and Current Plan Level Information
The information shown in this section captures the historical data for the twelve-month period used in the base period experience. This should be the same time period as the Experience Period found in Worksheet 1. See the instructions for Worksheet 1 for the definition of the Experience Period.
For small group submissions, the information in this section, except where noted, should reflect the Experience Period data on Worksheet 1. For example, if the Experience Period on Worksheet 1 is calendar year 2022, the information on this section should be for calendar year 2022.
2.2.2.1 Experience Period and Current Data
Issuers enter data for the Experience Period as well as current enrollment and premium in this section. The experience period entries are then used to calculate a loss ratio and PMPM amounts.
Allowed Claims: Enter the total allowed claims for each benefit plan with service dates within the Experience Period.
The Allowed Claims across all benefit plans for the Experience Period should be consistent with the Allowed Claims entered in Section I of Worksheet 1.
Reinsurance: Enter any claims reimbursement received through a federal or state reinsurance program, net of any reinsurance fees.
If the reinsurance recoveries during the Experience Period are not available at the time of the filing, issuers should enter their best estimate of the expected recoveries.
Member Cost Sharing: Enter any cost sharing (i.e., deductible, coinsurance, copayments) paid by the members. This should not include any cost sharing paid on behalf of the member through federal cost sharing reductions.
Cost Sharing Reduction: Enter any cost sharing paid on behalf of the member through federal cost sharing reduction subsidies.
If the federal government does not pay cost-sharing reduction subsidies, the amount entered here should be $0.
Incurred Claims: This is a calculated field that displays the incurred claims which the issuer is responsible for paying.
This field is automatically calculated by subtracting reinsurance, member cost sharing, and cost sharing reductions from allowed claims. Please check to make sure this amount reflects the incurred claims that are the issuer’s responsibility.
Risk Adjustment Transfer Amount: Enter the risk transfer payment or charge during the Experience Period for each plan.
Transfer amounts should include the high cost risk pool adjustment to claims and any assessment to pay for those claims. The risk adjustment user fee should not be included here, but rather in the taxes and fees portion of administrative costs. Payments made to an issuer from the risk adjustment program should be entered as a positive amount, while charges assessed to an issuer should be entered as a negative amount.
In some cases the risk adjustment payment or charge from the Experience Period may not be final. Issuers should provide their best estimate in these cases. As previously mentioned, risk adjustment should account for RADV adjustments, including DDVCs and allocations, as appropriate.
Premium: Enter the total premium earned in the Experience Period for each plan. See the instructions for Worksheet 1 for the definition of Experience Period Premium.
Experience Period Member Months: Enter the total number of months of coverage during the Experience Period for all members that had single risk pool coverage during any portion of the Experience Period.
For example, if a given member had coverage for five months during the Experience Period, that member would contribute five member months to the total member months for the period. The number entered must be an integer. For partial months, issuers should define a methodology for counting partial months and apply the methodology consistently to all members. Possible methodologies include but are not limited to rounding up, rounding down, rounding to nearest, and counting the member month if the member is active on the 15th of the month.
Current Enrollment: Enter a snapshot of the number of members currently enrolled in the plan as of a recent date. The date should be indicated in the actuarial memorandum (e.g., enrolled lives as of March 31, 20XX).
Tip:
Current Enrollment should be a recent snapshot of enrolled lives as
of a particular date in time (e.g., enrolled lives as of March 31,
20XX).
Current Premium PMPM: Enter the current premium PMPM amount for each plan. This should reflect the current population enrolled in the plan.
For small group quarterly rate filings, this should reflect the current premium of members affected by the rate filing. If the filing were effective October 1, the current premium would reflect the current premium for groups that will be renewing in the fourth quarter.
As with the current enrollment, the date used should be indicated in the actuarial memorandum. Again, some states may wish to establish a uniform date issuers should use.
Loss Ratio: This is a calculated field in the template that divides incurred claims by premium plus the risk adjustment transfer amount. This is not the federal MLR for determining rebates.
2.2.2.2 Per Member Per Month (PMPM) Calculations
This section of Worksheet 2 automatically calculates PMPM amounts for many of the Experience Period Data fields described above. Issuers should check the calculated PMPM amounts for reasonability, as an odd PMPM could indicate a data entry error.
Allowed Claims: This is a PMPM amount calculated by dividing allowed claims by Experience Period member months.
Reinsurance: This is a PMPM amount calculated by dividing reinsurance amounts by Experience Period member months.
Member Cost Sharing: This is a PMPM amount calculated by dividing member cost sharing amounts by Experience Period member months.
Cost Sharing Reduction: This is a PMPM amount calculated by dividing cost sharing reduction amounts by Experience Period member months.
Incurred Claims: This is a PMPM amount calculated by dividing incurred claim amounts by Experience Period member months.
Risk Adjustment Transfer Amount: This is a PMPM amount calculated by dividing risk adjustment amounts by Experience Period member months.
Premium: This is a PMPM amount calculated by dividing premium amounts by Experience Period member months.
2.2.3 Section III: Plan Adjustment Factors
The Plan Adjustment Factor section pulls the MAIR rate for the Projection Period from Worksheet 1 and applies the permitted plan-level adjustments to the Index Rate14 to calculate the PAIR. This section also collects the allowable calibration factors15 to calculate a Calibrated Plan Adjusted Index Rate. The Calibrated Plan Adjusted Index Rate can be thought of as a base rate where an individual’s premium could be calculated by applying the appropriate age rating factor, geographic rating factor, and tobacco use rating factor.
AV and Cost Sharing Design of Plan: Enter the allowable adjustment to the MAIR accounting for the actuarial value and cost sharing design of the plan.
This factor should not include adjustments that take into account the morbidity of the population expected to enroll in the plan.
Provider Network Adjustment: Enter the allowable adjustment to account for a plan’s provider network, delivery system characteristics, and utilization management practices.
This factor should only reflect differences between the network characteristics of the plan and the average network characteristics of all plans. The weighted average of the network factors for all plans should be 1.0.
Benefits in Addition to EHB: Enter the adjustment to the MAIR accounting for benefits the plan offers in addition to EHBs.
As the MAIR reflects allowed claims for EHBs only, this adjustment accounts for benefits provided in addition to EHBs. For individual market QHPs, CMS expects that “Benefits in Addition to EHB” is the multiplicative inverse of the “EHB Percent of Total Premium” field in the Plans & Benefits Template when rounded to the fourth decimal point (i.e., 1 divided by “EHB Percent of Total Premium"). As part of data integrity review, CMS will identify any mismatch between “Benefits in Addition to EHB” in the URRT and the reciprocal of “EHB Percent of Total Premium” in the Plans & Benefits Template and prompt you to confirm that the submitted values are correct.
Certain benefits, including routine non-pediatric dental services, routine non-pediatric eye exam services, long-term/custodial nursing home care benefits, and non-medically necessary orthodontia should not be considered EHB, even if the State EHB Benchmark plan covers such benefits.16
A state may require a QHP to offer benefits in addition to the EHB, but the state is required to defray the cost of such state-required benefits to the enrollee or to the QHP issuer on behalf of the enrollee.17 How an individual market QHP issuer should handle the portion of premium related to these services depends on whether the state makes these defrayal payments to the enrollee or to the issuer:
In a state that defrays the cost of a state-required benefit in addition to EHB directly to the QHP issuer:
The issuer should exclude the amount the state will defray (or that the state will begin defraying in the plan year for which the rates apply) from the rates submitted on both the URRT and the Rates Table Template.
The issuer should indicate in the Actuarial Memorandum that accompanies the URRT that the issuer anticipates the state will defray to the issuer the cost of any state-required benefit that is in addition to EHB and that, therefore, the cost of the state-required benefit is not included in the issuer’s rates in the URRT. QHP issuers should provide additional detail regarding the amount the QHP issuer expects to receive from the state for defrayal of the state-required benefit.
The issuer should not factor the state-required benefit into the calculation of “Benefits in Addition to EHB” (the multiplicative inverse the “EHB Percent of Total Premium” field in the Plans & Benefits Template).
This is because the QHP issuers should treat the state-required benefit as if it does not exist for purposes of the “EHB Percent of Total Premium” field, such that the state-required benefit is excluded from both the EHB percent of premium and the total premium from which the EHB percent of premium is calculated.
However, the QHP issuer should still indicate in the Benefits Information field on the Plans and Benefits template that it covers the state-required benefit in question as a non-EHB.
In a state that defrays the cost of a state-required benefit in addition to EHB directly to the enrollee:
The QHP issuer should include the amount the state defrays (or that the state will begin defraying in the plan year for which the rates apply) in the rates submitted on both the URRT as well as in the Rates Table Template.
The QHP issuer should indicate in the Actuarial Memorandum the amount that the issuer anticipates the state will defray directly to the enrollee for the cost of any state-required benefit that is in addition to EHB.
The QHP issuer should factor the state-required benefit into the calculation of “Benefits in Addition to EHB” (the multiplicative inverse the “EHB Percent of Total Premium” field in the Plans & Benefits Template).
This is because, although the QHP issuer should not include the state-required benefit in the EHB Percent of Total Premium on the Plans & Benefits Template, it should include the cost of the state-required benefit in the total premium from which the EHB Percent of Total Premium is calculated (therefore treating it as non-EHB for purposes of the total premium).
The QHP issuer should indicate in the Benefits Information field on the Plans and Benefits template that the QHP covers the state-required benefit in question as a non-EHB.
For plans that include coverage of abortion services for which public funding is prohibited (also known as non-Hyde abortion services)18 offered in states where the benefits package of the EHB benchmark plan includes such abortion services, you must handle the portion of the premium related to these services using one of the two methods described below:
If the plan is a QHP offered on an SBE or an FFE, do not include the percentage of the premium associated with such abortion services in the EHB percentage (even if these services are in the EHB benchmark package). The EHB percentage is used to calculate subsidy amounts and subsidy payments may not be provided for costs associated with such abortion services. Therefore, costs associated with such abortion must be excluded from the EHB proportion, and reflected accordingly in the adjustment for benefits in addition to EHB.
If the plan is not a QHP offered on an SBE or an FFE but is only offered off the Exchange, the percentage of the premium associated with abortion services for which public funding is prohibited may be included in the EHB percentage.
For plans that include coverage of abortion services for which public funding is permitted and that is offered in states where the benefits package of the EHB benchmark plan includes such abortion services, the plan should include the percentage of premium associated with these services in the EHB percentage.
For plans that include coverage of abortion services for which public funding is prohibited and that the plan is covering outside of the scope of the state’s EHB benchmark package, reflect any such covered abortion services as benefits in addition to EHB.
Administrative Expense: Enter the administrative expense portion of total administrative costs as a percent of the PAIR.
Taxes and Fees: Enter the taxes and fees portion of total administrative costs as a percent of the PAIR.
Exchange user fees should not be included in this percent, as those are already accounted for in the MAIR.
Profit & Risk Load: Enter the profit and risk load portion of total administrative expense as a percent of the PAIR.
Catastrophic Adjustment: For catastrophic plans only, enter the allowable adjustment for the expected eligibility categories for the plans. For non-catastrophic plans, enter a value of 1.0.
Issuers may consider the expected impact of specific eligibility categories for catastrophic plans. No adjustment is allowed on metal plans (platinum, gold, silver, or bronze) or the single risk pool index rate to account for a catastrophic plan adjustment. In other words, an issuer may not lower the rates of catastrophic plans due to an expectation that healthier members will choose these plans, then make up the revenue shortfall for this adjustment by increasing rates on the metal tier plans. While a separate plan-level adjustment is permitted for catastrophic members, catastrophic plan experience must be included in the single risk pool. Permitting an adjustment to metal plans to account for the catastrophic plan adjustment effectively excludes catastrophic plan experience from the single risk pool, which is not consistent with the single risk pool provision. In addition, the catastrophic adjustment should not duplicate the impact of age that is reflected by application of the standard age curve to the Calibrated Plan Adjusted Index Rate.
Plan Adjusted Index Rate: This field is automatically calculated in the spreadsheet by applying the permitted plan-level adjustments to the MAIR.
Age Calibration Factor: Enter the appropriate age calibration factor to calibrate the issuer’s actual population to an age rating factor of 1.0 so that multiplying by the appropriate age rating factor will result in the correct premium rate for a member of that age.
Note the URRT multiplies the PAIR by the age calibration factors, so issuers should be sure the calibration is entered as a multiplicative factor.
CMS will allow for the application of a factor of zero (0) for the distribution of members expected to pay no premium when developing the age calibration factor in states that follow the standard CMS age curve to account for the lost revenue due to the three under age 21 child dependent cap. While CMS is allowing this methodology, states with an Effective Rate Review Program that follow the standard CMS age curve may choose to allow or disallow this practice.
Some states have established their own age curves that are different from the standard CMS age curve. In this case, issuers should check with their state regulators to determine if applying a factor of zero (0) for the distribution of members expected to pay no premium is an appropriate and allowable adjustment for the three under age 21 child dependent cap.
Issuers must provide a detailed explanation of the methodology used in the calibration to the age curve. Specifically, issuers should describe the factors used in the determination of the age calibration factor, a description of the data used to weight the factors, and a description of the exact calculation. Issuers will need to provide actuarial justification that the methodology employed in the calculation of the average age and the calibration to the age curve complies with the standard age curve methodology.
Tip:
The age curve is not linear. Attempts to treat it as such when
performing the age curve calibration will likely result in
unexpected results.
Geographic Calibration Factor: Enter the appropriate geographic calibration factor to calibrate the issuer’s actual population to a geographic rating factor of 1.0 so that multiplying by the appropriate geographic area rating factor will result in the correct premium rate for a member (individual or enrolled with a group) located in that rating area.
The issuer must provide the geographic factor calibration that is applied to the projected single risk pool, if one is necessary. For example, if the weighted average of the geographic factors does not equal 1.0, calibration may be required.
The Actuarial Memorandum should explain how the geographic rating factor is calculated and state the rating factor only reflects differences in the costs of delivery (which can include unit cost and provider practice pattern differences) and not differences in population morbidity by geographic area.
Note that the geographic calibration adjustment is not plan specific. In other words, the same geographic calibration would be applied to all plans in the projected single risk pool.
Tobacco Calibration Factor: Enter the tobacco calibration factor that calibrates the issuer's actual population to a tobacco rating factor of 1.0 so that multiplying by the tobacco rating factor will result in the correct premium rate for a tobacco-using member.
Issuers using tobacco rating factors must calibrate the PAIR to remove the portion of the cost expected to be recouped through the tobacco surcharge. This adjustment should only reflect the expected surcharge collected for tobacco users. In the event tobacco users enter a wellness program which reduces the tobacco user load applied, only the net impact on revenue should be taken into account in the adjustment factor.
Calibrated Plan Adjusted Index Rate: This field is automatically calculated in the template by multiplying the PAIR by the age, geographic, and tobacco calibration.
The Calibrated Plan Adjusted Index Rate can be thought of as a base rate. Applying the appropriate age factor, geographic area factor, and tobacco use factor should result in the correct premium for a member or group enrolling on the effective date of the proposed rates.
Tip:
Calibration adjustments are applied uniformly to all plans.
Plan-specific calibrations are not allowed.
2.2.4 Section IV: Projected Plan Level Information
The information shown in this section captures the projected data for the twelve month period following the effective date for each plan. It is expected that in general, the Projection Period found in this section should be the same as the Projection Period found in Section II of Worksheet 1.
2.2.4.1 Projection Period Data
Issuers enter expected data for the Projection Period in this section. The entries are then used to calculate a loss ratio and PMPM amounts.
Allowed Claims: Enter the expected allowed claims for each benefit plan with service dates within the Projection Period.
Reinsurance: Enter any claims reimbursement received through a federal or state reinsurance program, net of any reinsurance fees.
Member Cost Sharing: Enter any cost sharing (i.e., deductible, coinsurance, copayments) expected to be paid by the members. This should not include any cost sharing paid on behalf of the member through federal cost share reductions.
Cost Sharing Reduction: Enter any cost sharing expected to be paid on behalf of the member through federal cost sharing reduction subsidies.
If the federal government does not pay cost-sharing reduction subsidies, the amount entered here should be $0.
Incurred claims: This is an automatically calculated field that displays the projected incurred claims which the issuer is responsible for paying.
This field is calculated by subtracting reinsurance, member cost sharing, and cost sharing reductions from allowed claims. Please check to make sure this amount reflects the incurred claims that are the issuer’s responsibility.
Risk Adjustment Transfer Amount: Enter the risk adjustment transfer payment or charge expected to be paid for the Projection Period for each plan.
Transfer amounts should include the high cost risk pool adjustment to claims and any assessment to pay for those claims. The risk adjustment user fee should not be included here, but rather in the taxes and fees portion of administrative costs. If the issuer expects to receive a projected risk adjustment payment, then the entry should be a positive value. If the issuer expects to owe a projected risk adjustment charge, then the entry should be a negative value.
Note that the reported risk adjustment transfer amounts should account for RADV adjustments, including DDVCs and allocations, as appropriate.
Premium: Enter the expected total premium earned in the Projection Period for each plan.
Projected Member Months: Enter the expected member months for each single risk pool plan in the Projection Period.
Loss Ratio: This is an automatically calculated field in the template that divides incurred claims by premium plus the risk adjustment transfer amount. This is not the federal MLR for determining rebates.
2.2.4.2 Per Member Per Month (PMPM) Calculations
This section of Worksheet 2 automatically calculates PMPM amounts for many of the Projection Period Data fields found above. Issuers should check the calculated PMPM amounts for reasonability, as an odd PMPM could indicate a data entry error.
Allowed Claims: This is a PMPM amount calculated by dividing allowed claims by Projected Member Months.
Reinsurance: This is a PMPM amount calculated by dividing reinsurance amounts by Projected Member Months.
Member Cost Sharing: This is a PMPM amount calculated by dividing member cost sharing amounts by Projected Member Months.
Cost Sharing Reduction: This is a PMPM amount calculated by dividing cost sharing reduction amounts by Projected Member Months.
Incurred Claims: This is a PMPM amount calculated by dividing incurred claim amounts by Projected Member Months.
Risk Adjustment Transfer Amount: This is a PMPM amount calculated by dividing risk adjustment amounts by Projected Member Months.
Premium: This is a PMPM amount calculated by dividing premium amounts by Projected Member Months.
Section 2.3 Worksheet 3 – Rating Areas
Worksheet 3 captures an issuer’s rating area factors for rating areas in which the issuer offers plans. Click on the “Create Rating Areas” button, then enter the total number of rating areas that are in the state, regardless of the number of rating areas where coverage will actually be offered. Beginning in Row 6, the issuer can identify the rating areas where coverage will be offered in Column A and enter the corresponding area rate factor in Column B.
For example, if a state had 8 rating areas and the issuer were to offer coverage in all of rating areas 1 and 3 and offer coverage in one county of rating area 5, the issuer would select 8 for the number of rating areas in the state. Beginning in cell A6, the issuer would select rating areas 1, 3, and 5 from the dropdown list in column A (select Rating Area 1 in cell A6, Rating Area 3 in cell A7, and Rating Area 5 in cell A8) and enter the appropriate rating factor in column B next to the corresponding rating area in column A. The issuer would not need to select the other rating areas in the state where coverage is not being offered by the issuer.
3. Part II: Written Description Justifying the Rate Increase
Part II is a brief, non-technical consumer-oriented explanation of the rate increase subject to review, intended to provide context for the quantitative information provided in Part I. This data should clearly explain the information given in Part I.
Accordingly, Part II should identify and explain the key drivers of the rate increase in Part I. For example, if inpatient costs are reported as the main factor of the rate increase, the written explanation should describe why hospital costs are increasing.
The explanation should include information on the following components related to the rate increase:
Scope and range of the rate increase: Provide the number of individuals impacted by the rate increase. Explain any variation in the increase among affected individuals (e.g., describe how any changes to the rating structure impact premium).
Financial experience of the product: Describe the overall financial experience of the product, including historical summary-level information on historical premium revenue, claims expenses, and profit. Discuss how the rate increase will affect the projected financial experience of the product.
Changes in Medical Service Costs: Describe how changes in medical service costs are contributing to the overall rate increase. Discuss cost and utilization changes as well as any other relevant factors that are impacting overall service costs.
Changes in benefits: Describe any changes in benefits and explain how benefit changes affect the rate increase. Issuers should explain whether the applicable benefit changes are required by law.
Administrative costs and anticipated margins: Identify the main drivers of changes in administrative costs. Discuss how changes in anticipated administrative costs and underwriting gain/loss are impacting the rate increase.
There is no standardized reporting form for Part II, but issuers are expected to cover the items listed above in their submissions. HIOS will require the issuer to enter Part II if any renewing plan within a product has a rate increase of 15% or more. The written statement must be uploaded in HIOS in one of the accepted document types. Such information posted by the issuer will be clearly displayed as the statements of the issuer. CMS will not edit the statements provided by issuers for Part II.
4. Part III: Actuarial Memorandum and Certification Instructions
The Part III Actuarial Memorandum instructions below are considered the minimum requirements for a Part III submission. However, issuers are encouraged to provide as much detail and supporting documentation as possible in advance to avoid delaying the review process. If additional information is necessary to properly complete the review, issuers are required to respond to all questions in a limited timeframe. Failure to provide information on a timely basis or failure to provide accurate information slows the review process and puts the issuer at risk for missing critical deadlines to offer products and plans in the individual, small group, and combined markets.
The Actuarial Memorandum must also capture appropriate actuarial certifications related to:
The methodology used to calculate the AV Metal Value for each plan.
The development of the Index Rate in accordance with federal regulations, and the development of plan specific premium rates using allowable modifiers to the Index Rate.
The geographic rating factors, which should reflect differences only in the costs of delivery (which can include unit cost and provider practice pattern differences) and not differences in population morbidity by geographic area.
State specific required information or certifications may also be included at the actuary’s discretion to avoid the need to create a separate state actuarial memorandum.
In any case where information provided is not broadly applicable to all products and plans included in the submission, please clearly indicate to which products and plans the information applies.
4.1 Redacted Actuarial Memorandum
As required by 45 CFR 154.215(h)(2), CMS will make available to the public the information contained in Part III of each Rate Filing Justification that is not a trade secret or confidential commercial or financial information, consistent with HHS FOIA regulations, 45 CFR 5.31(d). To facilitate release of Part III to the public, health insurance issuers must upload two versions of Part III: (1) a non-redacted version for CMS review (“CMS version”) and (2) a redacted version that will be made available to the public (“public version”). The CMS version should contain all data elements and information required in this manual with no redactions. The public version should redact only information that is a trade secret or confidential commercial or financial information. Redacted Actuarial Memorandums will be reviewed for compliance with 45 CFR 5.31(d) to ensure that issuers are not redacting more information than is allowable according to the regulation.
The HIOS system requires the Redacted Actuarial Memorandum to be uploaded to a particular field, or a box may be checked indicating CMS should use the non-redacted Actuarial Memorandum uploaded for CMS review. If an issuer selects this box, the non-redacted version will appear on the HHS website (RateReview.Healthcare.gov).
4.2 General Information Section
This section of the Actuarial Memorandum should include general information about the issuer and the policies which are the subject of the submission. The information provided in this section should include at least the following:
Company Identifying Information: Provide the following information that uniquely identifies the issuer submitting the memorandum. The information must be the same as the entries in the general information section of Worksheet 1 of the URRT (see the instructions for the URRT for additional definition of these fields):
Company Legal Name: the organization's legal entity name associated with the HIOS Issuer ID.
State: the state that has regulatory authority over the policies.
HIOS Issuer ID: the HIOS ID assigned to the legal entity.
Market: the market in which the products and plans are offered.
Effective Date: the effective date of the change of the Index Rate.
Company Contact Information: Provide the following information detailing how the reviewing regulator should contact the company in the case additional information is needed.
Primary Contact Name: Provide the name of the person at the company who will serve as the primary contact for the submission. The regulator will contact this person if there are questions related to the information submitted, or if additional information is needed.
Primary Contact Telephone Number: Provide the phone number for the primary contact.
Primary Contact Email Address: Provide the email address for the primary contact.
4.3 Proposed Rate Changes
In this section the actuary must provide the proposed rate change(s) and information related to the proposed rate change(s). If the proposed rate adjustment varies by product, the information provided should clearly identify which proposed adjustments apply to which products. Include all products which are part of the single risk pool, as defined by 45 CFR 156.80, including those products for which no rate adjustment is being proposed. The information that must be provided includes the following items:
Reason for Rate Increase(s): Provide the quantitative impact and a narrative description of all significant factors driving a proposed rate increase. As an example, these factors could include:
Single risk pool experience which is more adverse than that assumed in the current rates
Medical inflation
Increased utilization
Prospective changes to benefits covered by the product or successor products
New taxes and fees imposed on the issuer
Anticipated changes in the average morbidity of the covered population that is market-wide, as opposed to issuer specific morbidity that is reflected in risk adjustment
If the requested rate increase is not the same across all products and plans, provide an explanation as to why the rate changes vary by product or plan given they are based on the same single risk pool of experience for the market. Explain how the impact of morbidity was removed from impacting the variance in rate changes across products or plans.
4.4 Market Experience
The issuer is required to provide support that the single risk pool in a particular state and market is established according to the requirements in 45 CFR 156.80. The single risk pool reflects all covered lives for every non-grandfathered product/plan combination for an issuer in a state and market. The single risk pool is specific to the legal entity for the state and market for which it is submitted.
The single risk pool may include transitional products/plans for purposes of base rate experience used to demonstrate the single risk pool. The Projection Period should reflect experience of transitional policies to the extent the issuer anticipates the members in those policies will be enrolled in single risk pool plans during the Projection Period.
4.4.1 Experience and Current Period Premium, Claims, and Enrollment
This section of the Actuarial Memorandum should include information related to the actuary’s best estimate of premium, claims, and enrollment for the single risk pool during the Experience and Current Periods reported in Worksheet 1, Section I and Worksheet 2, Section II of the URRT.
Paid Through Date: Indicate the date through which payments have been made on claims incurred during the Experience Period.
Current Date: Provide the applicable date for which the current enrollment and premium is reported.
Allowed and Incurred Claims Incurred During the Experience Period: Provide support for the development of the actuary’s best estimate of allowed and paid claims incurred during the Experience Period.
Worksheet 1, Section I shows the actuary's best estimate of the amount of claims that were incurred during the 12-month Experience Period. Separately indicate the amount of claims which were processed through the issuer's claim system, processed outside of the issuer's claims system, and the amount that represents the actuary's best estimate of claims incurred but not reported as of the Paid Through Date stated above. This should be provided separately for Incurred Claims in Experience Period and Allowed Claims.
Describe the method used for determining Allowed Claims. For example, Allowed Claims could come directly from an issuer's claim records or alternatively could be developed by combining paid claims or capitation payments with member cost-sharing.
Provide support for the estimate of incurred but not reported claims.
Describe the methodology used to develop the estimate of claims incurred but not reported for both Allowed Claims and Incurred Claims in the Experience Period. To the extent that the methodology or completion factors used to estimate incurred but not reported claims on an allowed basis differs from the methodology or completion factors used to estimate incurred claims, describe and support why they are different.
Indicate whether the claims used to develop any completion factors reflect the Experience Period claims for the information submitted or some alternate claims set, such as a larger block of the issuer's experience. If an alternate claims set was used, please provide support for why it is appropriate.
If the incurred but not reported claims are unusually high or unusually low relative to the Experience Period claims paid as of the Paid Through Date, explain what is causing them to be unusually high or unusually low (e.g., introduction of a new claims system, significant employee turnover, etc.).
4.4.2 Benefit Categories
For each of the Benefit Categories in Worksheet 1, Section II, describe the methodology used to determine which category each claim in the Experience Period falls.
4.4.3 Projection Factors
This section should include a description of each factor used to project the Experience Period Index Rate to the Projection Period and supporting information related to the development of those factors. For each factor, the actuary should include a description of the source data or assumptions used, why they are appropriate for the single risk pool, and any applicable adjustments made to the data, such as considerations for issuer specific experience, industry or internal studies, benefit design, and credibility of the source data.
4.4.3.1 Trend Factors
Trend Factors (cost/utilization): Trend factors reported in the URRT are broken out by Year 1 and Year 2, as well as between cost and utilization. To calculate the Trended EHB Allowed Claims PMPM, the spreadsheet multiplies the Experience Period Index Rate PMPM by the trend factors entered.
For quarterly small group filings, the terms “Year 1” and “Year 2” are used loosely. Depending upon the Experience Period and Projection Period used, Years 1 and 2 might not cover a 12 month period. The trend rates entered should be the applicable trend that takes the Experience Period Index Rate to the MAIR for the effective date of the filing. For example, if an issuer were to file a third quarter rate increase, the trends entered should lead to a projected Index Rate and MAIR for July 1. Once the permitted plan-level adjustments and calibrations are applied, the Calibrated Plan Adjustment Index Rate should be the effective base rate for July 1. Applying the appropriate age, rating area, and tobacco use factors should generate consumer premium rates effective July 1.
As the trend factors entered in the URRT may not represent the annual trend number, the issuer should specify the annual trends and months of trend applied to Year 1 and Year 2 in the Actuarial Memorandum.
Demonstrate and describe the trend calculation, including source claims data used and methodology used for developing the cost and utilization projection factors, including all adjustments made to the data. Explain why the adjusted source data is applicable to the single risk pool. Some examples of such adjustments include, but are not limited to, the following:
Normalization for changes in age.
Normalization for benefit changes that occurred during the period (even if allowed claims are used to project trend, a normalization adjustment may be warranted to account for the influence that changes in benefits have on utilization).
Adjustments for seasonality patterns underlying the claims that may skew calculated trends.
Normalization for any one-time events which are not anticipated to reoccur during the Projection Period.
Adjustments for anticipated changes in provider contracts that differ from those underlying the experience used.
For prescription drugs, any adjustments made to account for changes in the formulary, expiration of patents, or introduction of new drugs.
4.4.3.2 Adjustments to Trended EHB Allowed Claims PMPM
This section should explain adjustments other than trend that are made to the Experience Period claims in order to develop the projected Index Rate.
Morbidity Adjustment: Describe any adjustment factors applied to the projected claims to account for anticipated differences in the average morbidity of the pooled population underlying the Experience Period and the issuer’s population anticipated to be insured in the Projection Period. These adjustments are shown in the “Morbidity Adjustment” entry on Worksheet 1, Section II. The morbidity of the population could be impacted by items such as guaranteed availability, an individual mandate to maintain coverage, expansion of Medicaid programs, and the introduction of a Basic Health Program.
Demographic Shift: Describe the development of the demographic shift factor used to adjust the projected claims to reflect differences between the average mix of the population by age, gender, and region underlying the base period experience and the average mix anticipated to underlie the Projection Period. Describe and support the age/gender factors underlying the development of these claims-based demographic adjustment factors.
Plan Design Changes: Describe the development of factors used to adjust the Experience Period claims to reflect the average benefits that will be covered during the Projection Period, including any newly mandated benefits (if any). The factors could adjust for items including but not limited to the following:
Addition of any benefits covered under the state EHB Benchmark Plan.
Any newly mandated benefits required under state law that are not reflected in the Experience Period claims.
Adjustment for the removal of benefits covered in the Experience Period claims that will not be covered in the Projection Period.
Anticipated changes in the average utilization of services due to differences in average cost- sharing requirements during the Experience Period and average cost-sharing requirements in the Projection Period.
Other Adjustments: Describe any other adjustments, in addition to morbidity, demographics, and plan design changes which are specifically addressed above, that are reflected in the “Other” adjustments entry on Worksheet 1, Section II. Also describe how these factors were developed. Some examples might include legislative changes affecting the market other than mandated benefits or changes brought about by State Relief and Empowerment Waivers under section 1332 of the ACA.
4.4.3.3 Manual Rate Adjustments
For issuers with Experience Period claims that are not determined to be fully credible, the use of other credible claims experience must be employed in developing a Manual EHB Allowed Claims PMPM for the Projection Period. The actuary must provide information related to the other experience and general methodology used in developing the manual rate.
Source and Appropriateness of Experience Data Used: State and describe the source data used to develop the manual rate and why such data is appropriate. Sources considered reasonable for developing manual rates include but are not limited to:
Multiple years of experience for the market for which rates are being submitted.
The issuer's experience for similar policies nationwide, including rationale for inclusion/exclusion of various blocks of business.
A manual rate developed by a consultant with appropriate supporting documentation as to the underlying source data for development of the manual rate.
Adjustments Made to the Data: The experience upon which the manual rate is based must be adjusted to reflect the population, region, provider network, and benefits anticipated under the policies for which rate increases are being submitted. Demonstrate and describe all adjustments made to the data underlying the development of the manual rate to account for differences in demographics, benefits, and morbidity/risk to ensure that the resulting manual rate is appropriate for blending with the adjusted Experience Period claims.
Inclusion of Capitation Payments: If some of the services in the Projection Period will be provided under a capitation arrangement, specifically demonstrate and describe how these payments were accounted for in the development of the credibility manual rate.
4.4.3.4 Credibility of Experience
In this section issuers must provide support for the credibility level assigned to their base period experience, with the complement being applied to a credibility manual rate. This includes items such as:
A description of the credibility methodology used.
The resulting credibility level assigned to the base period experience when applying the proposed credibility methodology.
When the base period experience is partially credible and included in experience used to develop the manual rate, the actuary must consider the extent to which the manual rate development double counts the base period experience. If the proposed manual rate lacks sufficient independence from the base period experience, the credibility percentage in the template should be adjusted such that the experience is assigned the appropriate credibility (based on the issuer’s credibility formula), taking into consideration the proportion of the manual experience that is from the subject base experience. In this case additional documentation should be included in the Actuarial Memorandum to demonstrate that the credibility factor applied in the template is consistent with the issuer’s credibility formula.
When determining credibility, the actuary should consider Actuarial Standard of Practice #25, “Credibility Procedures.”
4.4.3.5 Establishing the Index Rate
State the Index Rate following the specifications of 45 CFR 156.80(d)(1). The Index Rate is based on the total combined claim costs for providing EHBs only for the single risk pool of that state market. The Index Rate is derived by dividing the total combined EHB allowed claims for the single risk pool by all covered lives in the single risk pool of that state market. Issuers must establish a single Index Rate for all product/plan combinations in the single risk pool.
If the Experience Period contains non-single risk pool plans, provide the methodology used to develop the reported Experience Period Index Rate. Describe how claims for benefits which were covered during the Experience Period but are not EHBs were identified and removed.
Small Group Quarterly Trend Increases: State any scheduled small group quarterly trend adjustments to the index rate.
Small Group Quarterly Rate Filings: Rate adjustments for the small group market may be filed on a quarterly basis if permitted by the state. These quarterly filings may include adjustments for other items, such as new products, more recent Experience Period claims, etc. However, the rate development for these interim filings must be based on the single risk pool. The change in the Index Rate is only allowed to occur for the remainder of the calendar year, and a subsequent submission is required at the beginning of the next calendar year.
For example, if a small group issuer submits the URRT for January 1, they may submit a subsequent URRT that resets the Index Rate effective July 1 of that same year. The URRT effective July 1 in this example is only allowed to contain a trend increase for October 1 of that same year. Quarters after October 1 would be included in the next annual submission effective January 1 of the next calendar year.
4.4.3.6 Development of the Market-wide Adjusted Index Rate
Issuers are required to provide support for development of the MAIR, including an explanation for risk adjustment and exchange user fees entered in Worksheet 1 of the URRT. If state-based reinsurance information is entered in Worksheet 1 of the URRT, support for the development of the net reinsurance amount should also be provided.
The MAIR is calculated as the Index Rate adjusted for all allowable market-wide modifiers defined in the market rating rules, 45 CFR 156.80(d)(1). Since the Index Rate is on an allowed claims basis, the market level adjustments should be on an allowed basis.
The issuer is required to provide an explanation of how these modifiers are developed and applied to the Index Rate to develop the MAIR. Similar to the Index Rate, the MAIR reflects the average demographic characteristics of the single risk pool. In other words, the MAIR is not calibrated.
Reinsurance: Explain any expected reinsurance recoveries from federal or state reinsurance programs, net of the costs of the reinsurance, and the expected impact to claims in the Projection Period.
Risk Adjustment Payment/Charge: Under the single risk pool pricing requirements, issuers are required to make a market-wide adjustment to the pooled market-level Index Rate to account for federal risk adjustment payments and charges (including the high cost risk pool adjustment and any assessment to pay for those claims, but not risk adjustment user fees). Consistent with this adjustment, anticipated risk adjustment revenue must be allocated proportionally based on plan premiums for all plans within a risk pool by applying the risk adjustment transfer adjustment factor as a market-level adjustment. As previously mentioned, reported risk adjustment payment and charge amounts should account for RADV adjustments, including DDVCs and allocations, as appropriate.
Issuers must explain how they developed their estimated risk adjustment transfer amounts for all of the plans in the risk pool. Issuers are expected to explain all of their market and plan level assumptions related to the inputs of the HHS risk adjustment methodology (or alternative state methodology, if applicable). In other words, issuers must explain their assumptions related to plan-level and market-level risk scores and other relevant cost factor adjustments that are used to calculate payment transfers under the risk adjustment program. Issuers should explain any potential outlier assumptions that have a significant impact on transfers. Issuers may elect to provide supplemental exhibits detailing their plan-level transfer calculations in order to demonstrate that their transfer estimates appropriately track with the HHS payment transfer formula.
Issuers must also explain how the anticipated risk adjustment transfer amount was applied to the Index Rate in the development of the MAIR. Issuers should describe the overall impact of risk adjustment transfers on premiums.
Please note that the risk adjustment transfer amounts shown on Worksheet 1 of the URRT should take into account the actual PMPM amounts expected in the Projection Period. However, the risk adjustment transfer amount applied to the Index Rate in the development of the MAIR is on an allowed claims basis (i.e., prior to the application of the expected paid to allowed ratio) as the Index Rate is on an allowed claims basis.
Exchange User Fees: The issuer should provide a narrative verifying the Exchange user fees are applied as an adjustment to the Index Rate at the market level. A description of the process the issuer used to calculate the adjustment should be included. The value should reflect the expected mix of Exchange and non-Exchange enrollees.
4.4.4 Plan Adjusted Index Rate
The Plan Adjusted Index Rates for the Projection Period are included in Worksheet 2, Section III of the URRT.
The PAIR is calculated as the issuer’s MAIR adjusted for all allowable plan level modifiers defined in the market rating rules, 45 CFR 156.80(d)(2) and also entered in Section III of Worksheet 2 of the URRT. Only the following adjustments are allowable under these rules:
Actuarial value and cost-sharing design of the plan.
The plan's provider network, delivery system characteristics, and utilization management practices.
Benefits provided under the plan that are in addition to EHBs.
Administrative costs, excluding Exchange user fees and federal or state reinsurance fees (which are already accounted for in the MAIR). Section III of Worksheet 2 asks for the administrative costs broken out by Administrative Expense, Taxes and Fees, and Profit and Risk Load.
Only catastrophic plans may adjust for the expected impact of the specific eligibility categories for these plans. If an adjustment is made to catastrophic plans, this adjustment may not be recovered elsewhere in the rating process, as that would be seen as removing the catastrophic plan experience from the single risk pool.
Other adjustments not specified by 45 CFR § 156.80(d)(2) are not allowed at this point in the development, such as adjustments to recoup revenue related to the three under age 21 child dependent cap or a catastrophic adjustment to non-catastrophic plans.
The issuer is required to provide an explanation of how these modifiers are developed and applied to the MAIR to derive the PAIR.
The AV and cost-sharing design of the plan may take into account the benefit differences and utilization differences due to differences in cost-sharing. The utilization difference may reflect the impact higher cost-sharing has on utilization, but cannot reflect differences due to health status. If the cost-sharing impact on utilization is reflected, describe in detail how the difference was estimated and how the methodology ensures that differences due to health status are not included in the adjustment.
If benefits in addition to EHB are being provided, please describe the additional benefits.
Specifically, for the catastrophic plan rate, describe the methodology used to estimate the adjustment reflecting expected impact of the specific eligibility categories for these plans as compared to the single risk pool.
Similar to the Index Rate and MAIR, the PAIR reflects the average demographic characteristics of the single risk pool. In other words, the PAIR is not calibrated.
4.4.5 Calibration
Calibration factors are ONLY allowed for the age, geography, and tobacco factors.
Age Curve Calibration
Issuers must provide a detailed explanation of the methodology used in the calibration to the age curve. Specifically, issuers should describe the factors used in the determination of the calibration factor, a description of the data used to weight the factors, and a description of the exact calculation. Issuers will need to provide actuarial justification that the methodology employed in the calculation of the calibration to the age curve complies with the standard age curve methodology.
At this time CMS will allow for the application of a factor of zero (0) for the distribution of members expected to pay no premium when developing the age calibration factor in states that follow the standard CMS age curve to account for the lost revenue due to the three under age 21 child dependent cap. While CMS is allowing this methodology, states with an Effective Rate Review Program that follow the standard CMS age curve may choose to allow or disallow this practice.
Some states have established their own age curves that are different from the standard CMS age curve. In this case, issuers should check with their state regulators to determine if applying a factor of zero (0) for the distribution of members expected to pay no premium is an appropriate and allowable adjustment for the three under age 21 child dependent cap.
Include a demonstration of how the PAIR and the age curve are used to generate the schedule of premium rates for each plan. Note that the age curve calibration adjustment is not plan specific. In other words, the same age curve calibration must be applied to all plans in the projected single risk pool.
Geographic Factor Calibration
The issuer must provide the geographic factor calibration that is applied to the projected single risk pool, if one is necessary. For example, if the weighted average of the geographic factors does not equal 1.0, calibration may be required.
The Actuarial Memorandum must include a detailed description of the development of the geographic rating factors (including a description of how the methodology results in factors that reflect delivery cost differences only, or are otherwise adjusted for differences in population morbidity) and a demonstration of how these factors are applied to the PAIR. For example, if the weighted average of the geographic factors does not equal 1.0, the calibration adjustment that is applied should be included in the Actuarial Memorandum along with documentation of the calculation of the calibration adjustment. Note that the geographic calibration adjustment is not plan specific. In other words, the same geographic calibration would be applied to all plans in the projected single risk pool. If an issuer has multiple networks within a given rating area and wants to develop premiums specific for each network, the issuer must have a separate plan for each network within the rating area.
Tobacco Use Rating Factor Calibration
Issuers using tobacco rating factors must calibrate the PAIR to remove the portion of the cost expected to be recouped through the tobacco surcharge. This adjustment should only reflect the expected surcharge collected for tobacco users. In the event tobacco users enter a wellness program which reduces the tobacco user load applied, only the net impact on revenue should be taken into account in the adjustment factor.
Once the PAIR is calibrated to the 1.0 factor on the age curve and calibrated to the geographic rating area and tobacco use rating factors, the entire set of age rates is determined using the standard age factor of each age. The age factors must be the standard age curve set by HHS or a state specific age curve (if the state requires different age factors than the standard federal age curve).
4.4.6 Consumer Adjusted Premium Rate Development
The Actuarial Memorandum should describe how each allowable consumer level adjustment is applied to the PAIR so that the reviewing actuary can readily use the information to approximate Consumer Adjusted Premium Rates filed by the issuer.
The Consumer Adjusted Premium Rates are not displayed in the URRT.
4.5 Projected Loss Ratio
Indicate the projected loss ratio using the federally-prescribed MLR methodology. If the projected loss ratio is less than 80%, explain how the issuer plans to comply with the federal MLR requirement found in Public Health Service Act (PHS Act) section 2718.
If the state requires a projected loss ratio demonstration, then such a demonstration should also be included.
4.6 Plan Product Information
4.6.1 AV Metal Values
The issuer must describe whether the plan AV Metal Values included in Worksheet 2 of the URRT were calculated using only the AV Calculator or, if any plan designs are not compatible with the AV calculator, describe the acceptable alternative methodology used to generate the AV Metal Value. If an alternate methodology was used to develop the AV Metal Value(s), the actuary must provide a copy of the actuarial certification required by 45 CFR 156.135. The certification must be signed by a member of the American Academy of Actuaries and must indicate that the values were developed in accordance with generally accepted actuarial principles and methodologies.
The actuary must indicate the reason an alternate methodology was used, explain why the benefits for those plans for which an acceptable alternative methodology was used are not compatible with the AV Calculator, and state the chosen alternate methodology that was used for each applicable plan.
4.6.2 Membership Projections
Describe how the membership projections found in Worksheet 2 of the URRT were developed. Items impacting these projections could include, but are not limited to, changes in the size of the market due to introduction of guaranteed availability requirements (individual market), the individual mandate, expansion of Medicaid, and the introduction of a Basic Health Program.
Describe how projected member months by plan were developed relative to current membership by plan, and explain any differences.
For Silver level plans in the individual or combined markets, describe the methodology used to estimate the portion of projected enrollment that will be eligible for cost-sharing reduction subsidies at each subsidy level. State the resulting projected enrollment by plan and subsidy level.
4.6.3 Terminated Plans and Products
Include a list of terminated plans and any mappings to existing or new plans. List the name of each plan and product that will be terminated prior to the effective date. Include plans and products that have experience included in the single risk pool during the experience period and any products that were not in effect during the experience period but were made available thereafter. If a terminated plan will be mapped to a different plan in the projection period, the issuer must provide a cross-walk between the terminated plan(s) and the new plan(s).
4.6.4 Plan Type
In the event that the plan types listed in the drop-down box in Worksheet 2, Section I of the URRT do not describe an issuer’s plan exactly, and the issuer has selected the closest plan available, per the instructions, please describe the differences between the issuer’s plan and the plan type selected.
4.7 Miscellaneous Instructions
4.7.1 Effective Rate Review Information (Optional)
45 CFR 154.301 describes the elements of an Effective Rate Review Program. There are elements of an effective rate review for which the data needed to perform the review is not explicitly shown on the URRT (e.g., the health insurance issuer’s capital and surplus). Issuers may optionally provide additional information to facilitate an effective review of the submitted rate increase(s). While this information is optional, providing the information with the initial submission reduces the likelihood of the reviewer requesting supplemental information during the course of the rate review. In addition, states may have additional data requirements. Additional state-specific required data may be submitted with the URR submission.
4.7.2 Reliance
If, in preparing the URRT submission, the certifying actuary relied on any information or underlying assumptions provided by another individual, the information relied upon and the name of the individual providing that information should be disclosed.
4.7.3 Actuarial Certification
An actuarial certification must be provided for the following:
The methodology used to calculate the AV Metal Value for each plan.
The Index Rate is developed in accordance with federal regulations and the Index Rate along with allowable modifiers are used in the development of plan specific premium rates.
The geographic rating factors reflect only differences in the costs of delivery (which can include unit cost and provider practice pattern differences) and do not include differences for population morbidity by geographic area.
State-specific required information or certifications may also be included at the actuary’s discretion to prevent the need for creating multiple Actuarial Memorandums for the same filing. If an actuary chooses to exclude state-specific required information from the Actuarial Memorandum, this information would need to be provided to the state regulatory agency under separate cover.
The opining actuary must be a member of the American Academy of Actuaries, in good standing, and have the education and experience necessary to perform the work. The actuary must develop rates in accordance with the appropriate Actuarial Standards of Practice (ASOPs) and the profession’s Code of Professional Conduct. While other ASOPs apply, particular emphasis is placed on the following:
ASOP No. 5, Incurred Health and Disability Claims
ASOP No. 8, Regulatory Filings for Health Benefits, Accident and Health Insurance, and Entities Providing Health Benefits
ASOP No. 12, Risk Classification
ASOP No. 23, Data Quality
ASOP No. 25, Credibility Procedures
ASOP No. 26, Compliance with Statutory and Regulatory Requirements for the Actuarial Certification of Small Employer Health Benefit Plans
ASOP No. 41, Actuarial Communications
ASOP No. 50, Determining Minimum Value and Actuarial Value under the Affordable Care Act
At a minimum, the actuarial certification must include the following:
Identification of the certifying actuary and a statement that he/she is a member of the American Academy of Actuaries.
A certification that the projected Index Rate is:
In compliance with all applicable state and federal statutes and regulations (45 CFR 156.80 and 147.102)
Developed in compliance with the applicable Actuarial Standards of Practice
Reasonable in relation to the benefits provided and the population anticipated to be covered
Neither excessive nor deficient
A certification that the Index Rate and only the allowable modifiers as described in 45 CFR 156.80(d)(1) and 156.80(d)(2) were used to generate plan level rates.
A certification that the geographic rating factors reflect only differences in the costs of delivery (which can include unit cost and provider practice pattern differences) and do not include differences for population morbidity by geographic area.
A certification stating that the AV Calculator was used to determine the AV Metal Values shown in Part I of Worksheet 2 in the URRT for all plans except those specified in the certification. If an alternate methodology was used to calculate the AV Metal Value for at least one plan offered, a copy of the actuarial certification required by 45 CFR 156.135 must be included. The certification must be signed by a member of the American Academy of Actuaries and must indicate that the values were developed in accordance with generally accepted actuarial principles and methodologies.
For purposes of rate review, also include the reason an alternate methodology was used and the chosen alternate methodology that was used for each applicable plan. Describe the process that was used to develop the AV Metal Value.
The actuary may qualify the opinion, if desired, to state that the URRT does not demonstrate the process used by the issuer to develop the rates. Rather, it represents information required by federal regulation to be provided in support of the review of rate increases, for certification of Qualified Health Plans for Federally-facilitated Exchanges, and for certification that the Index Rate is developed in accordance with federal regulation and used consistently and only adjusted by the allowable modifiers.
5. HIOS Submission
5.1 HIOS Submission Statuses
URR submissions in HIOS undergo several changes in status during the course of the rate review process. The following table describes the various statuses and their associated meanings.
Table 1 HIOS Submission Statuses
Status |
Definition |
Additional Information |
Next Step |
Pre-Validation |
An issuer has successfully created a submission in HIOS. |
The issuer can revise the submission during the Pre-Validation stage.19 |
The issuer should validate the submission by checking the validation box on the submission summary page in HIOS. |
Record Validated20 |
The issuer has validated the submission.
Note: The validator (usually a manager at the insurance company) must have “validator” authority within HIOS. |
The submission is locked and cannot be revised.
Note: If the issuer needs to make revisions after validating the submission, the issuer must have the submission unlocked first. |
Rate increases not subject to rate review: If all plans within the submission have rate changes <15%, the regulator21 reviews the submission for completeness and for compliance with applicable rating rules.
Rate increases subject to review: If any plan within the submission has a rate increase that is ≥ 15%, the regulator checks that the submission has all the required information.
|
Pending Supplemental Materials |
A previously validated submission has been unlocked. |
The issuer can revise the submission during the Pending Supplemental Materials phase. |
The issuer should revise the submission. |
Supplemental Materials Received |
The issuer has revised a submission that was previously in the Pending Supplemental Materials status. |
The issuer can revise the submission during the Materials Received phase. |
The issuer must re-validate their submission. |
Rate Filing Accepted23 |
A submission not subject to rate review has passed the compliance review, and CCIIO has checked the “Web Content Assessment” box in HIOS. |
Only applicable to submissions where all plans have rate changes of < 15%. |
None. This is the final status for submissions not subject to rate review. |
Submission Filed |
CCIIO has checked the “Web Content Assessment” box in HIOS for a submission subject to rate review. |
Only applicable to submissions that contain a plan with a rate increase of ≥ 15%. |
The regulator must select “Review in Progress” in the dropdown menu in HIOS and then click Save. |
Review in Progress |
A submission subject to rate review is being reviewed by the regulator. |
Only applicable to submissions that contain a plan with a rate increase of ≥ 15%. |
The regulator must enter a Final Determination of Unreasonable or Not Unreasonable in HIOS. |
Review Complete24 |
The regulator has finished reviewing a submission subject to rate review and has entered a final determination of Not Unreasonable in HIOS. |
Only applicable to submissions that contain a plan with a rate increase of ≥ 15% that have been deemed Not Unreasonable. |
None. This is the final status for submissions with rate increases that are subject to rate review and have been determined by the regulator to be Not Unreasonable. |
Pending Final Justification |
The regulator has finished reviewing a submission subject to rate review and has entered a final determination of Unreasonable in HIOS. |
Only applicable to submissions that contain a plan with a rate increase of ≥ 15% that have been deemed Unreasonable. |
If the issuer decides to implement the Unreasonable rate increase, then the issuer must enter a Final Justification in HIOS.
If the issuer decides to modify the Unreasonable rate increase, the issuer should request a submission unlock and resubmit. If the issuer decides not to implement the unreasonable rate increase, then the issuer should contact CCIIO to request a submission deactivation. |
Final Justification Comments Submitted25 |
The issuer has entered a Final Justification in HIOS. |
Only applicable to submissions that contain a plan with a rate increase of ≥ 15% that have been deemed Not Unreasonable. |
None. This is the final status for submissions with rate increases that are subject to rate review, have been determined by the regulator to be Unreasonable, and will be implemented by the issuer. |
Submission Failed |
The issuer unsuccessfully attempted to create a submission in HIOS. |
Submission failures occur when the issuer enters invalid data or fails to enter required data. |
HIOS generates an email to the issuer indicating the submission failure. The issuer should create a new submission. |
Submission Deactivated |
CCIIO has deactivated the submission.
Note: In states with an Effective Rate Review Program, the state regulator must first contact CCIIO to request the deactivation. |
Only submissions with a status of Record Validated, Review Complete, or Rate Filing Accepted can be deactivated. |
The issuer should create a new submission. |
Pending Resubmission |
State Reviewer can request resubmission which puts the submission in “Pending Resubmission” status. |
Only applicable to submissions that contain a plan with a rate increase of ≥15% |
The issuer must revalidate submission and requires new content assessment by CMS. |
Pre-Validation Pending Part 2 Consumer Justification Narratives |
Issuer submitted a plan with a 15% or greater annual increase will result in HIOS identifying the product as subject to review and will require the issuer to enter a Consumer Justification Narrative for that product. |
Only applicable to submissions that contain a plan with a rate increase of ≥ 15%. |
The issuer must submit a Consumer Justification document on the Submit/Edit Consumer Justification Narratives section. |
Contractor Review in Progress |
CCIIO has assigned a submission to a Contractor to review |
Only applicable to submissions that contain a plan with a rate increase of ≥ 15%. |
The contractor needs to review and change status to Contractor Review Complete after they have completed their review |
Contractor Review Complete |
Contractor has completed their review. |
Only applicable to submissions that contain a plan with a rate increase of ≥ 15%. |
The contractor has finished their review. This is the final status for submissions with rate increases that are subject to rate review and have been sent to a contractor for review. |
5.2 Unlocking a Submission
If an issuer needs to change a previously validated submission for any reason (e.g. the regulator requests additional documentation, the issuer realizes that a file is missing), the issuer must first have the previous submission unlocked by the state or CCIIO.
The issuer must re-validate the submission after making revisions.
6. SERFF Submission
Tip:
The new system connection is Not Applicable to States without an
Effective Rate Review Program, or states that do not participate in
SERFF. Issuers in these states should continue to submit filings
directly into the HIOS URR module.
![]()
Tip:
Grandmothered plans, student health insurance coverage, and excepted
benefit products, such as stand-alone dental products, should not be
submitted through the SERFF transfer system connection.
Once the URRT has been uploaded, it will be automatically sent to CMS for validation and a message appears to the issuer in SERFF. Once the validation request has been processed, the message will update accordingly. If the validation is successful, SERFF will display the regenerated Excel file.
Issuers will be required to upload the Actuarial Memorandum and Redacted Actuarial Memorandum in the URRT tab. These two files must have different file names.
Issuers can upload the Consumer Justification Narrative (CJN) in the URRT tab regardless of if the filing meets the threshold making it subject to review, but if the filing is above threshold, upload of the CJN becomes a requirement.
An “Additional Supporting Documentation” section is available on the URRT tab in which up to 30 files can be uploaded.
The template and supporting URR items may also have the following SERFF functions applied, but these functions will not be transferred to the URR module of HIOS:
Request Confidentiality
Objections/Objections Letters
Change Schedule Items
Response Letters
Amendment Letters
State Public Access
Once the state review is complete, the state will need to close out the filing in SERFF. If the filing contains only plans below the threshold, the state regulator will mark the filing as “complete.” If the filing contains at least one plan above the threshold, the state regulator will enter a final determination. The state’s final determination and associated comments will be sent to the URR Module of HIOS and displayed on ratereview.healthcare.gov. Once a determination has been sent to CMS, there can be no further action on the URRT tab from the issuer or the state.
If changes need to be made to a filing after it has been put into a final status, the state must contact a member of the Rate Review team at CCIIO to have the submission deactivated in HIOS.27 The issuer must then start from scratch and create a new submission in SERFF. We strongly recommend that state regulators do not close out filings until they are certain that no further changes are necessary.
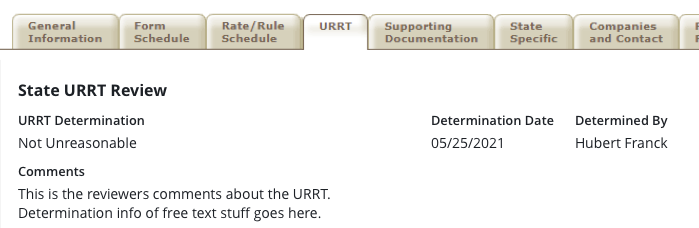
PRA Disclosure Statement
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is 0938-1140. This information collection is used to facilitate review of rate filings from issuers to determine if the proposed rate change is compliant with federal rating rules and if the proposed rate change is an increase that meets or exceeds the federal threshold, whether such an increase is unreasonable. The information on proposed and final rate changes are made publicly available to increase transparency and to allow for public comments on proposed rate increases. The time required to complete this information collection is estimated to average approximately 10 hours per response, including the time to review instructions, gather the data needed, and complete and review the information collection. This information collection is mandatory for issuers of non-grandfathered health insurance coverage in the individual and small group markets (45 CFR part 154). The information contained in each Rate Filing Justification collected that is not considered a trade secret or confidential commercial or financial information, will be made available to the public at https://ratereview.healthcare.gov/. Issuers are required to submit redacted actuarial memorandums for public display. If you have comments concerning the accuracy of the time estimate(s) or suggestions for improving this form, please write to: CMS, 7500 Security Boulevard, Mail Stop C4-26-05, Attention: Information Collections Clearance Officer Baltimore, Maryland 21244-1850 or keith.mcnamara@cms.hhs.gov.
1 The phrases “single risk pool plan” and “single risk pool coverage” are used to describe non-grandfathered health insurance coverage in the individual or small group (or combined) market that is subject to all of the single risk pool provisions at 45 CFR 156.80.
2 See 45 CFR 154.301. The current list of states that do not have an Effective Rate Review Program is available at https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/rate_review_fact_sheet.
3 45 CFR 5.31(d)
4 45 CFR 154.301(b)(1)(i)
5 45 CFR 154.301(b)(1)(ii)
6 For all instances in this document that refer to filing in the URR Module of HIOS, rate filing documentation that is filed through the NAIC’s System for Electronic Rate & Form Filing (SERFF) and automatically uploaded to the URR module of HIOS will be considered as filed with CMS. This filing option is not available for states that do not have an Effective Rate Review Program and states that do not participate in SERFF. For information on states with an Effective Rate Review Program, see https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/rate_review_fact_sheet. For information on state participation in SERFF, see https://www.serff.com/serff_participation_map.htm.
7 The Final Bulletin is available at https://www.cms.gov/cciio/resources/regulations-and-guidance#Review-of-Insurance-Rates
8 Health insurance issuers are required to submit rate filings for coverage that has been renewed under CMS’s non-enforcement policy continually since 2014. See Bulletin: Extension of Limited
Non-Enforcement Policy through 2023 and Later Benefit Years (March 23, 2022), available at: https://www.cms.gov/files/document/extension-limited-non-enforcement-policy-through-calendar-year-2023-and-later-benefit-years.pdf.
9 For more information on excepted benefits, see 45 CFR 146.145 and 148.220.
10 45 CFR 156.80(d)(3)
11 Approved state-specific rating variations are published on the CCIIO website at https://www.cms.gov/CCIIO/Programs-and- Initiatives/Health-Insurance-Market-Reforms/state-rating.html
12 https://www.cms.gov/CCIIO/Programs-and-Initiatives/Health-Insurance-Market-Reforms/state-rating.html
13 The URRT is required for single risk pool plans that experience rate increases (of any size), no rate changes, rate decreases, as well as new single risk pool plans.
14 45 CFR 156.80(d)(2)
15 45 CFR 156.80(d)(3)
16 45 CFR 156.115(d)
17 45 CFR 155.170
18 45 CFR 156.280(d)
19 Revising a submission means that the issuer can upload supplemental documents or revise the URRT or Actuarial Memorandum in HIOS.
20 This submission status also applies to SERFF submissions.
21 In states with an Effective Rate Review Program, the applicable state regulatory authority is the regulator. In states without an Effective Rate Review program, CCIIO is the regulator.
22 State regulators in states with an Effective Rate Review Program must notify CCIIO when a submission passes the compliance review.
23 This submission status also applies to SERFF submissions.
24 This submission status also applies to SERFF submissions.
25 This submission status also applies to SERFF submissions.
26 For information on states with an Effective Rate Review Program, see https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/rate_review_fact_sheet. For information on state participation in SERFF, see https://www.serff.com/serff_participation_map.htm
27 A member of the rate review team at CCIIO can be reached by emailing ratereview@cms.hhs.gov.
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| Author | Brent Plemons |
| File Modified | 0000-00-00 |
| File Created | 2024-09-05 |
© 2026 OMB.report | Privacy Policy