1 Survivors of Torture (SOT) Integrated Care Continuum (IC
Generic for ACF Program Monitoring Activities
SOT-ICC instrument
OMB: 0970-0558
OMB Control Number: 0970-0558
 Expiration
Date: 11/23/2023
Expiration
Date: 11/23/2023
Survivors of Torture Integrated Care Continuum (SOT-ICC)
The SOT-ICC Instrument was developed by the Center for Victims of Torture with support from the NCB project partners, Harvard Program for Refugee Trauma and NYU/Bellevue Program for Survivors of Torture. The NCB technical assistance project is funded by the U.S. Office of Refugee Resettlement (ORR) through cooperative agreement number 90ZT0142.
Introduction and Purpose
The Survivors of Torture Integrated Care Continuum instrument (SOT-ICC) is a self-assessment of integrated care practices and systems designed for programs delivering services to torture survivors.
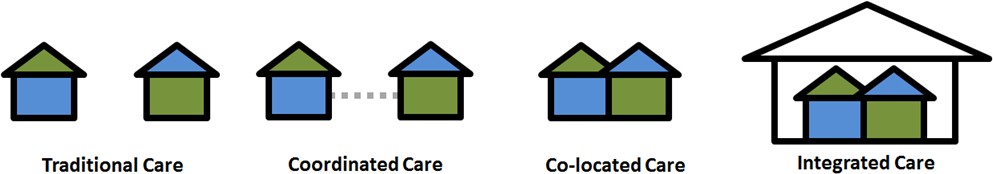
Multidisciplinary services may be delivered through different levels of integration. The Integrated Care Continuum (ICC) includes four levels ranging from minimal coordination of services (Traditional Care) and systems to full integration of services and systems (Integrated Care). The icons and descriptions below show the four levels of integration on the continuum.
The purpose of the SOT-ICC instrument is for program staff to discuss and identify the program’s position on the integrated care continuum and find opportunities for moving towards the program's optimal position on the continuum.
-
Separate facilities
Separate systems
Rare communication
about clients
Separate facilities
Separate systems
Occasional communication
about clients
Some shared facilities
Some shared systems
Regular communication
about clients
Fully shared facilities
Fully shared systems
Frequent communication
about clients
Who should self-assess using the SOT-ICC
We encourage programs to complete the SOT-ICC if they meet the following criteria:
Currently provide more than one discipline of services (e.g. psychological and social work, medical and psychological, legal and social work, etc.) to torture survivors.
Have an interest in learning about how to coordinate multiple types of services for torture survivors.
Benefits of self-assessment using the SOT-ICC
This assessment can help your program:
Build community, shared understanding, and shared vision for your program team
Learn together about the core components of integrated care and how they can be addressed within programs
Share diverse perspectives from across your program
Decide on concrete next steps towards your optimal level of integration on the continuum
Provide a useful structure and set time for valuable strategic thinking
Guidance on administration
In order to gain the greatest benefits from this self-assessment we recommend the following practices. Please see the following paragraphs for more information about each of these suggested practices.
Clearly defining the target of the self-assessment
Selecting a group of no more than 12 participants that bring a wide range of relevant perspectives to the discussion
Scheduling two 90 min sessions for all of your chosen participants, well in advance, and communicating that attendance is a priority
Designating a facilitator and a note-taker for the discussion sessions
Asking participants to review the self-assessment tool ahead of time
Deciding on follow-up or next steps as a group, even if the next step is to reconvene the discussion.
Defining the target of the self-assessment
The SOT-ICC is designed to be a self-assessment of level of integration within a specific program. The tool asks questions about the program within three domains: Program Develoment, Treatment Delivery, and If your organization has multiple programs with unique approaches to service delivery, each program should complete its own self-assessment as a group. In smaller organizations, this may mean that the whole organization completes one self- assessment if a consistent service delivery approach is utilized.
Selecting participants for the group discussion
The SOT-ICC is intended to be used in a group discussion format. To reap the benefits of this self-assessment, the discussion process should include a wide range of perspectives. This includes, for example, representatives from each provider discipline, managers/supervisors, administrative staff, support staff, and ideally individuals and/or families who receive or have received services from your program. Involving staff in different positions and with different experiences improves the potential for programs to identify high impact next steps.
The size of the group discussion depends on the size and nature of the program. We recommend that no more than 12 staff participate in order to keep the discussion focused and productive. If your program is too large to include all staff, we suggest nominating representatives that can speak to the different program disciplines and domains (program development, program logistics, and treatment delivery).
This tool does not work as intended if it is completed by an individual, or completed by many individuals separately who then average their results.
Planning time for the group discussion
The SOT-ICC takes between two and four hours to complete, depending on the size and discussion style of the group. We recommend planning two sessions of at least 90 minutes with a consistent group of participants. Previous participants have recommended scheduling and prioritizing time for these sessions far in advance. If it is not feasible to schedule ninety minutes, programs may break the task into shorter sessions with a consistent group of participants. This approach may be less disruptive to normal work activities; however, a disadvantage is there may also be less continuity to the conversation.
Roles for the self-assessment process
Each program should designate a facilitator and a note taker. The facilitator should read or present the written version of each item (by sharing screens, projecting, or having each person present review their own copy) and ask the group to suggest the response they think makes most sense for each item and why. It is important that the facilitator communicate and demonstrate that everyone’s opinion and perspective counts equally in the discussion. The group should work together to determine what response best matches their program. The factiliator will also need to pace the timing of the discussion to complete all required items within the allotted time period. The notetaker should, at a minimum, record the group’s selected responses and other important notes from the discussion.
Review the tool
We strongly recommend that staff are given at least a week’s time to review the SOT-ICC tool itself in advance of the group discussion in order to think about their possible responses. This preparation may benefit the whole group by allowing the discussion to be more productive and efficient. We suggest that the program manager or the self-assessment facilitator should email the document to all participants approximately a week before the first discussion session.
Next steps
A key outcome of completing the SOT-ICC is the collective learning experience for the program that program staff or leaders could use to inform an action-oriented improvement plan. The notes sections included can be used to record ideas for next steps for the program, or even questions that need to be answered related to integrated care. When you have completed the self-assessment, we recommend deciding on next steps as a team. Examples could include convening another discussion, reviewing the client database system, deciding on a new means of communication across disciplines, researching options for shared program space, etc.
Survivors of Torture Integrated Care Continuum (SOT-ICC)
The SOT-ICC Instrument was developed by the Center for Victims of Torture with support from the NCB project partners, Harvard Program for Refugee Trauma and NYU/Bellevue Program for Survivors of Torture. The NCB technical assistance project is funded by the U.S. Office of Refugee Resettlement (ORR) through cooperative agreement number 90ZT0142.
About your program and the SOT-ICC process
Fill out the following before or after the discussion process.
Dates on which SOT-ICC discussion process took place:
Which staff were present for the SOT-ICC discussion process? (list names and roles below)
Organization Name:
Program Name (if different):
Program Location (City, State):
Number of clients served by your program in the last 12 months (approximate): Number of staff in your program:
Which of the following services does your program provide survivors of torture?
Psychological
Legal
Medical
Social
Other:
Which of the following services does your program coordinate care with?
Psychological
Legal
Medical
Social
Other:
Programs have different visions for the level of integration that they feel is best or most appropriate for their situation or the needs of their clients. In your program’s long-term vision, which level of integration would your program optimally provide for the services that you provide and coordinate?
Traditional Care: Separate facilities & systems, rare communication about clients
Coordinated Care: Separate facilities & systems, occasional communication about clients
Co-located Care: Some shared facilities & systems, regular communication about clients
Integrated Care: Fully shared facilities & systems, frequent communication about clients
Survivors of Torture Integrated Care Continuum (SOT-ICC)
The SOT-ICC Instrument was developed by the Center for Victims of Torture with support from the NCB project partners, Harvard Program for Refugee Trauma and NYU/Bellevue Program for Survivors of Torture. The NCB technical assistance project is funded by the U.S. Office of Refugee Resettlement (ORR) through cooperative agreement number 90ZT0142.
Integrated Care Continuum Items:
Each numbered items in the sections below introduces a particular content area. The response options under that item are possible descriptions for how a program functions in that content area, organized by level of integration.
For each numbered content area, mark the one response option that discussion participants agree best describes your program right now. Include any notes for your own reference (about next steps, questions you have, etc.) in the side bar boxes on the right of the page.
 Part
1: Program
Development
Part
1: Program
Development
Program vision guides how a program will address complex conditions and needs of clients through multidisciplinary services.
[Traditional Care] Program vision is to deliver services through separate disciplines or agencies
[Coordinated Care] Program vision is to coordinate services between multiple disciplines or agencies
[Co-located Care] Program vision is to deliver multidisciplinary services in collaboration within close geographic proximity
[Integrated Care] Program vision is to deliver fully integrated multidisciplinary services
Funding structures determine resources and capacity of a program to deliver integrated care for clients.
[Traditional Care] Fundraising efforts are separate across disciplines/agencies and funds are allocated separately; no communication and coordination to avoid duplicative efforts in applying for funding (e.g. no joint grants or proposals)
[Coordinated Care] Separate budgets with different costs for each discipline/agencies; limited coordination on fundraising efforts across disciplines/agencies to avoid duplicative efforts
[Co-located Care] Shared fundraising goals and shared budget, strategizing of fundraising efforts based on programmatic fit, and funds are allocated to different disciplines/agencies
[Integrated Care] Fundraising goals and budgets are reciprocally shared across disciplines/agencies and funds are allocated to integrated teams
 Ongoing
training promotes
capabilities and
competencies of
staff in
understanding how
to care
for the
complex conditions
and needs
of clients.
Ongoing
training promotes
capabilities and
competencies of
staff in
understanding how
to care
for the
complex conditions
and needs
of clients.
[Traditional Care] Staff receive continuing education or training in their primary discipline only
[Coordinated Care] Staff receive continuing education or training in coordination of multidisciplinary services for shared clients
[Co-located Care] Staff receive continuing education or training in coordination of multidisciplinary services in the same location
[Integrated Care] Staff receive continuing education or training that is focused on building a shared understanding of interdisciplinary care in the same location
Understanding of expectations allows staff to comprehend what role they play in caring for the complex conditions and needs of clients.
[Traditional Care] Staff are informed of expectations and roles in their primary discipline only
[Coordinated Care] Staff are informed of expectations and roles in communication with other providers about shared clients
[Co-located Care] Staff are informed of expectations and roles in coordination of multidisciplinary services delivered at the same location
[Integrated Care] Staff are informed of expectations and roles in delivering interdisciplinary services through teams
There is at least one recognized champion who visibly initiates, supports, and sustains program vision to address complex conditions and needs of clients through integrated care is crucial.
[Traditional Care] There are recognized champion[s] who support and motivate staff to deliver their primary discipline area with excellence
[Coordinated Care] There are recognized champion[s] who support and motivate staff to communicate with other providers about shared clients
[Co-located Care] There are recognized champion[s] who support and motivate staff to coordinate multidisciplinary services in the same location
[Integrated Care] There are recognized champion[s] who support and motivate staff to deliver services through a shared interdisciplinary team in the same location
 Part
2: Program
Logistics
Part
2: Program
Logistics
Clinic management provides guidelines on policies and procedures for administrative systems.
[Traditional Care] Administrative systems are managed separately for each discipline
[Coordinated Care] Efforts are made to coordinate administrative paperwork and policies across disciplines as needed
[Co-located Care] Efforts are made to coordinate administrative paperwork and policies across providers who are delivering multidisciplinary services at the same location
[Integrated Care] Coordination of administrative paperwork and policies for a shared team of providers delivering interdisciplinary services is an integral part of care
Coordination of appointments promotes client access to services that address complex conditions and needs.
[Traditional Care] Scheduling system does not allow appointments to be coordinated between different providers on the same day
[Coordinated Care] Efforts are made to coordinate appointments with different providers on the same day but at different locations as needed by client
[Co-located Care] Efforts are made to coordinate appointments with different providers on the same day at the same location as needed by client
[Integrated Care] Coordination of appointments with different providers [or a team of providers] on the same day at the same location is an integral part of care
Language support in the primary language of clients is available to support scheduling of appointments and understanding of paperwork.
[Traditional Care] Limited language support over the phone is available to assist clients with scheduling and paperwork
[Coordinated Care] Limited in person interpreter support is available to assist clients with scheduling and paperwork; over the phone language support is used when in person interpreters are unavailable
[Co-located Care] Regular in person interpreter support is available to assist clients with scheduling and paperwork
[Integrated Care] In person interpreter support is available to assist clients with scheduling and paperwork as an integral part of care
 Part
3: Treatment
Delivery
Part
3: Treatment
Delivery
Documentation of client information facilitates shared understanding of client background and treatment progress among providers.
[Traditional Care] Client records are documented and accessible only to the discipline/provider that collects the information
[Coordinated Care] Client records are documented and maintained by each discipline separately and limited information from client records is shared between providers
[Co-located Care] Client records are documented through separate disciplines and shared between providers to deliver services at the same location
[Integrated Care] Client records are documented and maintained through interdisciplinary teams. Team members have full access for coordination and service delivery as an integral part of care
Treatment planning involves identifying a whole person treatment approach to address the complex conditions and needs of clients.
[Traditional Care] Each provider develops separate treatment plan for the client related to provider’s practice only
[Coordinated Care] Each provider develops separate treatment plan that consider the client’s complex needs in minimal collaboration with the other providers caring for the client
[Co-located Care] Each provider develops separate treatment plans that consider the client’s complex needs in close collaboration with the other providers caring for the client
[Integrated Care] Providers collaborate with one another as a team to develop an integrated treatment plan that addresses complex needs of the client
 Assessment
about the specific conditions and needs in multidisciplinary
areas (psychological,
medical, social,
legal) is
conducted to inform treatment planning and delivery.
Assessment
about the specific conditions and needs in multidisciplinary
areas (psychological,
medical, social,
legal) is
conducted to inform treatment planning and delivery.
[Traditional Care] Each provider assesses for conditions/needs related to their separate practice only
[Coordinated Care] Each provider assesses for conditions/ needs related to their discipline and results are shared as needed to coordinate care with other providers caring for the client
[Co-located Care] Each provider assesses for conditions/needs related to their discipline and there is a system for regularly sharing results to other providers caring for the client in close geographic proximity
[Integrated Care] A multidisciplinary team of providers works together to assess complex conditions/needs and there is a formalized system for sharing results among the team to inform collaborative, whole person care
Coordination of interventions between providers promotes complementary services to meet a client’s complex conditions and needs and limits the risk of service duplication.
[Traditional Care] Each provider delivers intervention separately with no coordination on service delivery across disciplines
[Coordinated Care] Each provider delivers interventions separately with limited coordination between providers of complementary services
[Co-located Care] Close coordination between providers to deliver complementary [yet distinct] interventions separately at the same location
[Integrated Care] Services are delivered through teams trained to deliver a range of services across multiple disciplines
There are systems in place for providers to discuss how to care for clients’ complex conditions and needs.
[Traditional Care] Systems in place do not provide access to consultation with providers outside of discipline
[Coordinated Care] Systems in place provide minimal or spontaneous access to consultation with providers outside of discipline for urgent client needs
[Co-located Care] Systems in place provide access to consultation with providers outside of discipline to coordinate on site services
[Integrated Care] Systems in place provide access to consultation among shared team of providers to holistically care for clients through the provision of multidisciplinary care
 Provider
motivation and
workflow determines
the time
and space that
providers have to collaborate on services to heal clients’
complex conditions and needs.
Provider
motivation and
workflow determines
the time
and space that
providers have to collaborate on services to heal clients’
complex conditions and needs.
[Traditional Care] Collaboration across disciplines is up to providers to initiate on their own time or as workflow allows
[Coordinated Care] Collaboration across disciplines is driven by the need to have more information on client cases
[Co-located Care] Collaboration across disciplines is driven by appreciation of onsite availability and referrals
[Integrated Care] Collaboration across disciplines is an integral part of workflow in order to treat and care for whole person
Closing of care takes into consideration ongoing conditions and needs of clients and how this may impact the need for continued services.
[Traditional Care] Decision to close services is approached separately by each provider
[Coordinated Care] Decision to close services is communicated with other providers caring for the client but closure processes are addressed separately by each provider
[Co-located Care] Decision to close services is determined in coordination with providers caring for the client in close geographic proximity
[Integrated Care] Decision to close services is formally assessed by a team of providers who work together to determine the client’s remaining need for multidisciplinary services
PAPERWORK REDUCTION ACT OF 1995 (Pub. L. 104-13) STATEMENT OF PUBLIC BURDEN: The purpose of this information collection is to assess the type of program model utilized by recipients and their progress in moving through the continuum. Public reporting burden for this collection of information is estimated to average 4 hours per grantee, including the time for reviewing instructions, gathering and maintaining the data needed, and reviewing the collection of information. This is a mandatory collection of information (HHS-2022-ACF-ORR-ZT-0051). An agency may not conduct or sponsor, and a person is not required to respond to, a collection of information subject to the requirements of the Paperwork Reduction Act of 1995, unless it displays a currently valid OMB control number. The OMB # is 0970-0558 and the expiration date is 11/30/2023. If you have any comments on this collection of information, please contact Margaret Brewinski-Isaacs at margaret.brewinskiisaacs@acf.hhs.gov or 202-821-9594.
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| Author | Maria Vukovich |
| File Modified | 0000-00-00 |
| File Created | 2023-08-30 |
© 2026 OMB.report | Privacy Policy