Form 0920 C4P Provider DCE Survey
Preferences for Longer-Acting Preexposure Prophylaxis (PrEP) Methods Among Persons in US Populations at Highest Need: A Discrete Choice Experiment
Att 8 Provider DCE Survey
C4P Provider DCE Survey
OMB: 0920-1400
Form Approved
OMB No. 0920-New
Expiration Date: XX/XX/XXXX
Preferences for Longer-Acting Preexposure Prophylaxis (PrEP) Methods Among Persons in US Populations at Highest Need: A Discrete Choice Experiment
Attachment #8
Provider DCE Survey
Public reporting burden of this collection of information is estimated to average 20 minutes per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing the collection of information. An agency may not conduct or sponsor, and a person is not required to respond to a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing this burden to CDC/ATSDR Reports Clearance Officer; 1600 Clifton Road NE, MS D-74, Atlanta, Georgia 30333; Attn: OMB-PRA (0920-New)
C4P DCE Provider Survey
Survey link: https://survey.rti.org/SE/1/ProviderSurveyDev
Note: text in blue indicate instructions for programming.
** Indicates item used to assess eligibility
U Indicates single response option only in question allowing multiple responses
Participants will be able to skip questions that they prefer not to answer; if a question on screen is not answered and the participant selects to move forward in the survey, the survey will note to the participant that an item is not answered and confirm if they would like to move forward and leave the question unanswered. The survey will code this response as a refusal.
Main Survey
We thank you for your interest in this survey and appreciate your time.
The survey will take approximately 20 minutes and is designed to be completed in one sitting. If you are not able to take 20 minutes now, we recommend you come back when you have enough time.
 As
a reminder, here is key information about the study and your rights.
As
a reminder, here is key information about the study and your rights.
Title of the research study: Choices for Prevention (C4P)
Principal Investigator: Dr. Sarah Roberts, RTI International
Study Sponsor: The Centers for Disease Control and Prevention (CDC) Division of HIV Prevention
KEY INFORMATION
You are invited to participate in a research study funded by the Centers for Disease Control and Prevention (CDC) and conducted by a non-profit research organization named RTI International.
Participation in this study is completely voluntary. You may choose not to take part in the study or leave the study at any time without any consequences.
The purpose of this research study is to understand provider preferences for several new long-acting PrEP, or pre-exposure prophylaxis, methods and how factors related to PrEP delivery might influence the decision to prescribe long-acting PrEP. PrEP is an HIV medication that people without HIV can take to prevent getting HIV from sex or injection drug use.
We will also ask you some direct questions about your opinions of different PrEP products and some more detailed questions about your background and experiences with PrEP. The survey should take about 20 minutes to complete.
All participants that complete the online survey will receive a $20 Visa gift card. The $20 gift card may be withheld if it is determined that you do not meet the eligibility criteria, you do not complete the survey, or there is evidence of fraud.
You may be uncomfortable answering some questions about yourself. You do not have to answer any questions that make you uncomfortable.
The study has a minimal level of risk. The key risk is small chance of a loss of confidentiality. To help minimize this risk you will be assigned a unique research ID number. Additionally, your personally identifying information (e.g., name, email address) will be kept separate from your data and will only be accessible to the research staff at RTI International.
Several long-acting Pre-exposure prophylaxis (PrEP) products are currently in development or have recently been approved by the FDA.
We would like to ask you about your opinions of these products and about what factors related to PrEP delivery are most important to you when choosing to prescribe PrEP.
We will ask you to compare different hypothetical PrEP options and think about which one you would prefer to prescribe. The options will be described by 5 independent characteristics or factors. Each option presented to you will have a different combination of the 5 factors.
We will first describe each of the 5 factors. The first describes different long-acting PrEP products. We will then present other factors of PrEP delivery that we would like you to consider.
Please go to the next screen.
Product Type
The new long-acting PrEP products may come in different forms and be dosed with different frequency.
Each product has some potential side effects. In clinical trials conducted to date, nearly all side effects were graded as mild (causing no or minimal interference with usual social & functional activities with intervention not indicated) or moderate (causing greater than minimal interference with usual social & functional activities with intervention indicated) in severity.
Because most of these products are still being studied, information on possible side effects may beincomplete. Other important details about product administration are also still unknown. For the purposes of this study, please assume:
The products have similar efficacy (over 99% reduction in HIV risk), grace periods for missed doses, and lab monitoring requirements.
For all products, clients will have to come to the clinic for HIV and STI testing at least every 3-6 months
There is no evidence of drug interactions between PrEP and other common medications, including birth control or hormones
All products may be recommended for any person reporting sexual behaviors or drug injection practices that place them at substantial ongoing risk of HIV exposure and acquisition, regardless of gender, sexual identity, or source of HIV exposure.
Please go to the next screen.
Monthly Oral Pill
The
first product is an oral pill taken once every month. 
In
a phase II study with 242 participants, the most common side effects
were:
Nausea
in 5%
Diarrhea
in 5%
Headache
in 9%
These
typically resolved within a few weeks after participants started to
take the pill.
Implant
The next product is a subcutaneous implant that lasts for 12 months.
The implant is placed under the skin of the patient’s non-dominant upper arm using an applicator. It would have to be removed and replaced by a health care provider after 12 months, or could be taken out early, if desired.
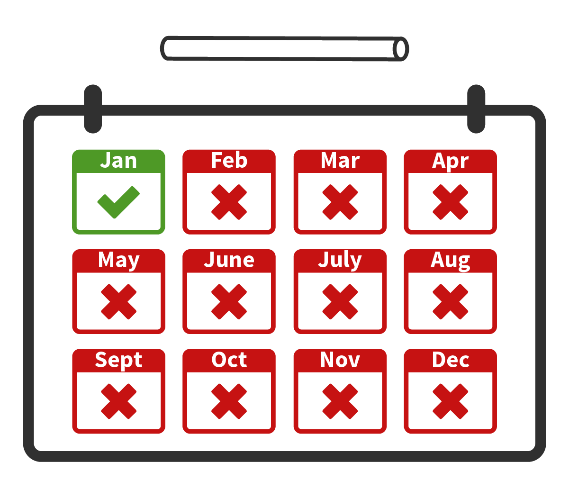
In
two phase I studies with 52 total participants, the most common side
effects were:
Temporary
implant-site reactions in 67%
hematoma,
swelling, itching, induration, tenderness/pain
Headache
in 17%
These
typically resolved within 4 weeks of insertion.
Have you ever performed an insertion of a subcutaneous implant (contraception, treatment of opioid dependency, hormone therapy, or other indications)?
Yes, please describe: _________________
No
Injection
Another product is an injection into the gluteal muscle every 2 months.
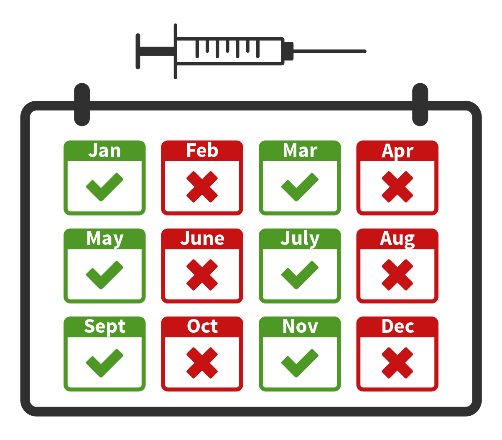
In two phase III studies with 7,789 total participants, the most common side effects were:
Temporary injection site reactions in (81% in one study, 32% in the other):
Pain or discomfort, tenderness, swelling, and/or nodules at the location of the injection
These
typically lasted for a few days after the injection and decreased in
frequency with subsequent injections received over time.
Two Injections
The last product is two injections administered subcutaneously into the abdomen every 6 months.

No studies have been completed of this product as an HIV prevention method; however, Phase III studies are underway. In two studies of these injections as treatment for people living with HIV, the most common side effects were:
Temporary injection site reactions in 50%:
Pain or discomfort, tenderness, swelling, and/or small nodules at the location of the injection.
Most of these reactions resolved a few days after receiving the injections. The nodules lasted for several months in some participants, but were mild and were palpable but not visible.
To summarize, the table below lists each possible long-acting PrEP product type with the most common side effects from studies to date.
Product Type Potential Temporary Side Effects |
|
|---|---|
Oral pill every 1 month
|
In a phase II study with 242 participants, the most common side effects were:
These typically resolved 2-3 weeks after product initiation.
|
Implant every 12 months
|
In two phase I studies with 52 total participants
These typically resolved within 4 weeks of insertion.
|
Injection every 2 months
|
In two phase III studies with 7,789 total participants
These typically lasted for a few days after each injection
|
Two injections every 6 months
|
In two studies of these injections as treatment for people living with HIV:
Most resolved a few days after receiving the injections. The nodules lasted for several months in some participants, but were mild and were palpable but not visible. |
How willing would you be to prescribe each of the following long-acting PrEP products if you gained the required training, knowledge, and skills to do so?
|
Not at all |
A little |
Somewhat |
Very |
Extremely |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Next, we will describe other factors of PrEP delivery that we would like you to think about. As a reminder, our goal is to understand your preferences for providing any of these PrEP methods to your patients. One factor is the type of PrEP product, but there are other factors of PrEP delivery that may influence your willingness to prescribe PrEP.
In what follows, we will describe the following other potential factors that are considered as part of the 5 PrEP characteristics in this survey:
Out-of-pocket costs for your patient
Training needed to support product administration
Initial time required from all clinic staff (for first prescribing appointment)
Reimbursement for your services
Please read these descriptions carefully. This information will help you answer the questions later in the survey.
Please go to the next screen.
Out-of-Pocket Costs for Patient
Some patients can have co-pay or co-insurance cost for PrEP covered through health plans. If a patient is uninsured or out-of-pocket-costs are high, there are assistance programs that can help, but patients might still be expected to pay some amount.
If a patient uses a long-acting PrEP product for one year, their out-of-pocket costs could vary. We will ask you to consider two cost scenarios: no out-of-pocket costs (free); and $50 per month ($600 per year).
Patient Out-of-Pocket Costs |
|
|---|---|
Free, $ 0 per year ($ 0 per month)
|
The long-acting PrEP product would be free of cost for your patient, $0 per year. |
$ 600 per year ($ 50 per month)
|
The long-acting PrEP product would cost your patient $ 50 per month or $ 600 per year. |
Training on Products and PrEP Needs Assessment
As new PrEP options become available, the training required to gain the knowledge and skills to prescribe or deliver the product could vary. Training could be one 1-hour session, providing only information about the product and administration and standard guidance on assessing indications for PrEP with patients; or it could be two 1-hour sessions, with the second hour focused onincreasing comfort or competence in discussing potential exposures to HIV with your patients, including sexual behavior and injection drug use practices, the potential benefits of PrEP for avoiding HIV infection, and their interest in PrEP.
In this survey we would like you to consider 2 training options.
Training would only need to be completed once before you could begin prescribing to patients:
Training Prior to First Administration |
|
|---|---|
1
hour; standard |
One hour session covers information about the PrEP product and administration (including skills needed to deliver the product) and routine training on how to assess PrEP indications with patients. |
2 hours; standard + enhanced patient interactions
|
Two sessions, each 1 hour (2 hours total), covering the PrEP product and administration plus enhanced training to increase comfort or competence in discussing potential HIV exposure, sexual behavior and injection drug use practices, and interest and benefits of PrEP use. |
How comfortable are you currently with discussing need for HIV prevention and interest in oral PrEP with your patients?
Very comfortable
Somewhat comfortable
Somewhat uncomfortable
Very uncomfortable
Length of Initial Evaluation
The initial appointment to prepare a patient to start PrEP could require varying amounts of time from you and/or your clinic staff, for example, to complete eligibility screening, counseling, consult with the patient about potential side effects, complete insurance or assistance program paperwork, and interpret lab work.
For this survey, we would like you to consider 3 possibilities for first appointment times.
Time Required for Initial Evaluation |
|
|---|---|
30 minutes
|
The first appointment would require 30 minutes of clinic staff time. |
60 minutes
|
The first appointment would require 60 minutes of clinic staff time. |
75 minutes
|
The first appointment would require 75 minutes of clinic staff time. |
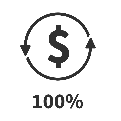
Reimbursement
Your clinic may receive different levels of reimbursement for the HIV prevention services billed to a patient’s insurance or covered by a grant (e.g., from the Health Resources & Services Administration Health Center Program).
We would like you to think about two possibilities:
Reimbursement |
|
|---|---|
Partial, 60%
|
You receive 60% reimbursement for the HIV prevention services provided to your patient |
Full, 100%
|
You receive 100% reimbursement for the HIV prevention services provided to your patient |
Thinking About Prescribing Long-Acting PrEP
Suppose your patient wants to start taking a medication to help prevent themself from getting HIV. HIV antigen/antibody and RNA lab tests confirm that the patient is HIV-negative, and the patient’s medical history is otherwise unremarkable. The patient is currently using condoms consistently for HIV prevention.
Assume your clinic has the ability to provide all of the long-acting PrEP methods we have described previously. In addition, assume that for this patient, the risk of side effects are the same.
In the next 11 questions, we will show you different pairs of hypothetical long-acting PrEP options, each described by 5 independent factors of PrEP delivery.
For each question:
Please consider the PrEP options presented in each table, reviewing each characteristic, and choose the one that you would prescribe.
The 2 options will be different in each question.
Please assume your clinic has the ability to provide all of these options.
If you don’t like either option, you can select “I would not prescribe either of these methods.”
There are no right or wrong answers; we are interested in your personal opinion.
NOTE: Each participant will be randomly assigned to a version (of 8 possible).
They will answer 10 questions from their assigned version. All participants will see one additional question (called fixed choice set).
The following 10 questions are an example of the types of questions the participant will be asked to complete, but do not represent the exact
|
Which of the following HIV prevention options would you prefer to prescribe? 1/ 10Factor |
PrEP Option A |
PrEP Option B |
Neither |
|
Product Type |
Implant Every 12 months
|
Every 2 months
|
I would not prescribe either of these methods
|
|
Patient’s Out-of-Pocket Costs |
Free, $ 0 per year ($ 0 per month) |
$ 600 per year ($ 50 per month) |
|
|
Training Prior to First Administration |
1 hour; standard |
2 hours; standard + enhanced patient interactions |
|
|
First Appointment Length |
60 minutes
|
30 minutes
|
|
|
Reimbursement |
Full, 100%
|
Partial, 60% |
|
|
|
|
|
|
|
Which PrEP option would you prescribe? |
|
|
|
Which of the following HIV prevention options would you prefer to prescribe? 2/ 10
|
Factor |
PrEP Option A |
PrEP Option B |
Neither |
|
Product Type |
|
every 12 months |
I would not prescribe either of these methods
|
|
Out-of-Pocket Costs |
Free, $ 0 per year ($ 0 per month) |
$ 600 per year ($ 50 per month) |
|
|
Training Prior to First Administration |
1 hour; standard |
2 hours; standard + enhanced patient interactions |
|
|
First Appointment Length |
30 minutes |
75 minutes |
|
|
Reimbursement |
Full, 100% |
Partial, 60% |
|
|
|
|
|
|
|
Which PrEP option would you prescribe? |
|
|
|
Which of the following HIV prevention options would you prefer to prescribe? 3/ 10
|
Factor |
PrEP Option A |
PrEP Option B |
Neither |
|
Product Type |
|
Oral pill every 1 month |
I would not prescribe either of these methods
|
|
Out-of-Pocket Costs |
$ 600 per year ($ 50 per month) |
Free, $ 0 per year ($ 0 per month) |
|
|
Training Prior to First Administration |
1 hour; standard |
2 hours; standard + enhanced patient interactions |
|
|
First Appointment Length |
75 minutes |
60 minutes |
|
|
Reimbursement |
Partial, 60% |
Full, 100% |
|
|
|
|
|
|
|
Which PrEP option would you prescribe? |
|
|
|
Which of the following HIV prevention options would you prefer to prescribe? 4/ 10
|
Factor |
PrEP Option A |
PrEP Option B |
Neither |
|
Product Type |
every 12 months |
every 2 months |
I would not prescribe either of these methods
|
|
Out-of-Pocket Costs |
$ 600 per year ($ 50 per month) |
Free, $ 0 per year ($ 0 per month) |
|
|
Training Prior to First Administration |
1 hour; standard |
2 hours; standard + enhanced patient interactions |
|
|
First Appointment Length |
60 minutes |
30 minutes |
|
|
Reimbursement |
Partial, 60% |
Full, 100% |
|
|
|
|
|
|
|
Which PrEP option would you prescribe? |
|
|
|
Which of the following HIV prevention options would you prefer to prescribe? 5/ 10
|
Factor |
PrEP Option A |
PrEP Option B |
Neither |
|
Product Type |
Oral pill every 1 month |
|
I would not prescribe either of these methods
|
|
Out-of-Pocket Costs |
$ 600 per year ($ 50 per month) |
Free, $ 0 per year ($ 0 per month) |
|
|
Training Prior to First Administration |
1 hour; standard |
2 hours; standard + enhanced patient interactions |
|
|
First Appointment Length |
75 minutes |
60 minutes |
|
|
Reimbursement |
Full, 100% |
Partial, 60% |
|
|
|
|
|
|
|
Which PrEP option would you prescribe? |
|
|
|
Which of the following HIV prevention options would you prefer to prescribe? 6/ 10
|
Factor |
PrEP Option A |
PrEP Option B |
Neither |
|
Product Type |
every 2 months |
every 12 months |
I would not prescribe either of these methods
|
|
Out-of-Pocket Costs |
$ 600 per year ($ 50 per month) |
Free, $ 0 per year ($ 0 per month) |
|
|
Training Prior to First Administration |
1 hour; standard |
2 hours; standard + enhanced patient interactions |
|
|
First Appointment Length |
60 minutes |
30 minutes |
|
|
Reimbursement |
Full, 100% |
Partial, 60% |
|
|
|
|
|
|
|
Which PrEP option would you prescribe? |
|
|
|
Which of the following HIV prevention options would you prefer to prescribe? 7/ 10
|
Factor |
PrEP Option A |
PrEP Option B |
Neither |
|
Product Type |
every 2 months |
every 12 months |
I would not prescribe either of these methods
|
|
Out-of-Pocket Costs |
Free, $ 0 per year ($ 0 per month) |
$ 600 per year ($ 50 per month) |
|
|
Training Prior to First Administration |
Two sessions, 4 hours; administration + patient interactions |
One session, 2 hours; administration only |
|
|
First Appointment Length |
75 minutes |
30 minutes |
|
|
Reimbursement |
Partial, 60% |
Full, 100% |
|
|
|
|
|
|
|
Which PrEP option would you prescribe? |
|
|
|
Which of the following HIV prevention options would you prefer to prescribe? 8/ 10
|
Factor |
PrEP Option A |
PrEP Option B |
Neither |
|
Product Type |
Oral pill every 1 month |
|
I would not prescribe either of these methods
|
|
Out-of-Pocket Costs |
Free, $ 0 per year ($ 0 per month) |
$ 600 per year ($ 50 per month) |
|
|
Training Prior to First Administration |
1 hour; standard |
2 hours; standard + enhanced patient interactions |
|
|
First Appointment Length |
75 minutes |
60 minutes |
|
|
Reimbursement |
Partial, 60% |
Full, 100% |
|
|
|
|
|
|
|
Which PrEP option would you prescribe? |
|
|
|
Which of the following HIV prevention options would you prefer to prescribe? 9/ 10
|
Factor |
PrEP Option A |
PrEP Option B |
Neither |
|
Product Type |
|
Oral pill every 1 month |
I would not prescribe either of these methods
|
|
Patient’s Out-of-Pocket Costs |
Free, $ 0 per year ($ 0 per month) |
$ 600 per year ($ 50 per month) |
|
|
Training Prior to First Administration |
1 hour; standard |
2 hours; standard + enhanced patient interactions |
|
|
First Appointment Length |
75 minutes |
30 minutes |
|
|
Reimbursement |
Full, 100% |
Partial, 60% |
|
|
|
|
|
|
|
Which PrEP option would you prescribe? |
|
|
|
Which of the following HIV prevention options would you prefer to prescribe? 10/ 10
|
Factor |
PrEP Option A |
PrEP Option B |
Neither |
|
Product Type |
every 2 months |
every 12 months |
I would not prescribe either of these methods
|
|
Patient’s Out-of-Pocket Costs |
Free, $ 0 per year ($ 0 per month) |
$ 600 per year ($ 50 per month) |
|
|
Training Prior to First Administration |
1 hour; standard |
2 hours; standard + enhanced patient interactions |
|
|
First Appointment Length |
75 minutes |
30 minutes |
|
|
Reimbursement |
Full, 100% |
Partial, 60% |
|
|
|
|
|
|
|
Which PrEP option would you prescribe? |
|
|
|
Fixed choice task: all participants should see this question
Which of the following HIV prevention options would you prefer to prescribe?
|
Feature |
PrEP Option A |
PrEP Option B |
Neither |
|
Product Type |
every 2 months |
every 12 months |
I would not prescribe either of these methods
|
|
Patient’sCost to Patient |
Free, $ 0 per year ($ 0 per month) |
$ 600 per year ($ 50 per month) |
|
|
Training Prior to First Administration |
1 hour; standard |
2 hours; standard + enhanced patient interactions |
|
|
First Appointment Length |
60 minutes |
75 minutes |
|
|
Reimbursement |
Partial, 60% |
Full, 100% |
|
|
|
|
|
|
|
Which PrEP option would you prescribe? |
|
|
|
Now, we will ask your opinion about PrEP care for specific types of patients.
Daniel is a 31-year-old, Black man who is HIV-negative.
He currently has one [randomize sex of partner: half see “male,” half see “female”] sex partner, who has been diagnosed as HIV-positive and with whom he is monogamous. During previous appointments, you have discussed HIV risk with him and encouraged him to use condoms. However, he does not always use them.
He says that he wants to start taking a medication to help prevent himself from getting HIV. He has insurance that would cover the cost of the prescription.
His medical history is otherwise unremarkable. He has no physical complaints. HIV antigen/antibody and RNA lab tests confirm that he is HIV-negative.
How willing would you be to prescribe daily oral PrEP for Daniel?
-
Not at all willing
A little willing
Somewhat willing
Very willing
Extremely willing
How willing would you be to prescribe a PrEP injection every 2 months for Daniel if you gained the required training, knowledge, and skills to do so?
-
Not at all willing
A little willing
Somewhat willing
Very willing
Extremely willing
As a reminder:
Daniel is a 31-year-old, Black man who is HIV-negative.
He currently has one [male /female] sex partner, who has been diagnosed as HIV-positive and with whom he is monogamous. During previous appointments, you have discussed HIV risk with him and encouraged him to use condoms. However, he does not always use them.
He says that he wants to start taking a medication to help prevent himself from getting HIV. He has insurance that would cover the cost of the prescription.
His medical history is otherwise unremarkable. He has no physical complaints. HIV antigen/antibody and RNA lab tests confirm that he is HIV-negative.
How adherent do you think Daniel would be to taking a PrEP pill every day (daily oral PrEP)?
-
Not at all adherent
A little adherent
Somewhat adherent
Very adherent
Extremely adherent
As a reminder:
Daniel is a 31-year-old, Black man who is HIV-negative.
He currently has one [male /female] sex partner, who has been diagnosed as HIV-positive and with whom he is monogamous. During previous appointments, you have discussed HIV risk with him and encouraged him to use condoms. However, he does not always use them.
He says that he wants to start taking a medication to help prevent himself from getting HIV. He has insurance that would cover the cost of the prescription.
His medical history is otherwise unremarkable. He has no physical complaints. HIV antigen/antibody and RNA lab tests confirm that he is HIV-negative.
How adherent do you think Daniel would be to returning to clinic for a PrEP injection every two months?
-
Not at all adherent
A little adherent
Somewhat adherent
Very adherent
Extremely adherent
As a reminder:
Daniel is a 31-year-old, Black man who is HIV-negative.
He currently has one [male /female] sex partner, who has been diagnosed as HIV-positive and with whom he is monogamous. During previous appointments, you have discussed HIV risk with him and encouraged him to use condoms. However, he does not always use them.
He says that he wants to start taking a medication to help prevent himself from getting HIV. He has insurance that would cover the cost of the prescription.
His medical history is otherwise unremarkable. He has no physical complaints. HIV antigen/antibody and RNA lab tests confirm that he is HIV-negative.
How likely would Daniel be to have more condomless sex if he started taking PrEP?
-
Not at all likely
A little likely
Somewhat likely
Very likely
Extremely likely
As a reminder:
Daniel is a 31-year-old, Black man who is HIV-negative.
He currently has one [male /female] sex partner, who has been diagnosed as HIV-positive and with whom he is monogamous. During previous appointments, you have discussed HIV risk with him and encouraged him to use condoms. However, he does not always use them.
He says that he wants to start taking a medication to help prevent himself from getting HIV. He has insurance that would cover the cost of the prescription.
His medical history is otherwise unremarkable. He has no physical complaints. HIV antigen/antibody and RNA lab tests confirm that he is HIV-negative.
Alexa is a 28-year-old, [randomize race: half see “Black,” half see “White”] woman who is HIV-negative. She says that she wants to start taking a medication to help prevent herself from getting HIV and has insurance that would cover the cost of the prescription.
Alexa is in a committed relationship, she only has one male sex partner, but she does not know his HIV status and is uncertain about her partner’s fidelity. During previous appointments, you have discussed HIV risk with her and encouraged her to ask her partner to use condoms. However, she is not always able to convince him to use them, and reports having unprotected sex with her partner.
HIV antigen/antibody and RNA lab tests confirm that she is HIV-negative.She has previously been treated for STDs and her medical history is otherwise unremarkable.
How willing would you be to prescribe daily oral PrEP for Alexa?
-
Not at all willing
A little willing
Somewhat willing
Very willing
Extremely willing
How willing would you be to prescribe a PrEP injection every 2 months for Alexa if you gained the required training, knowledge, and skills to do so?
-
Not at all willing
A little willing
Somewhat willing
Very willing
Extremely willing
As a reminder:
Alexa is a 28-year-old, [Black /White] woman who is HIV-negative. She says that she wants to start taking a medication to help prevent herself from getting HIV and has insurance that would cover the cost of the prescription.
Alexa is in a committed relationship, she only has one male sex partner, but she does not know his HIV status and is uncertain about her partner’s fidelity. During previous appointments, you have discussed HIV risk with her and encouraged her to ask her partner to use condoms. However, she is not always able to convince him to use them, and reports having unprotected sex with her partner.
HIV antigen/antibody and RNA lab tests confirm that she is HIV-negative, though she has previously been treated for STDs. Her medical history is otherwise unremarkable.
How adherent do you think Alexa would be to taking a PrEP pill every day (daily oral PrEP)?
-
Not at all adherent
A little adherent
Somewhat adherent
Very adherent
Extremely adherent
As a reminder:
Alexa is a 28-year-old, [Black /White] woman who is HIV-negative. She says that she wants to start taking a medication to help prevent herself from getting HIV and has insurance that would cover the cost of the prescription.
Alexa is in a committed relationship, she only has one male sex partner, but she does not know his HIV status and is uncertain about her partner’s fidelity. During previous appointments, you have discussed HIV risk with her and encouraged her to ask her partner to use condoms. However, she is not always able to convince him to use them, and reports having unprotected sex with her partner.
HIV antigen/antibody and RNA lab tests confirm that she is HIV-negative, though she has previously been treated for STDs. Her medical history is otherwise unremarkable.
How adherent do you think Alexa would be to returning to the clinic for a PrEP injection every two months?
-
Not at all adherent
A little adherent
Somewhat adherent
Very adherent
Extremely adherent
As a reminder:
Alexa is a 28-year-old, [Black /White] woman who is HIV-negative. She says that she wants to start taking a medication to help prevent herself from getting HIV and has insurance that would cover the cost of the prescription.
Alexa is in a committed relationship, she only has one male sex partner, but she does not know his HIV status and is uncertain about her partner’s fidelity. During previous appointments, you have discussed HIV risk with her and encouraged her to ask her partner to use condoms. However, she is not always able to convince him to use them, and reports having unprotected sex with her partner.
HIV antigen/antibody and RNA lab tests confirm that she is HIV-negative, though she has previously been treated for STDs. Her medical history is otherwise unremarkable.
How likely would Alexa be to have more condomless sex if she started taking PrEP?
-
Not at all likely
A little likely
Somewhat likely
Very likely
Extremely likely
As a reminder:
Alexa is a 28-year-old, [Black /White] woman who is HIV-negative. She says that she wants to start taking a medication to help prevent herself from getting HIV and has insurance that would cover the cost of the prescription.
Alexa is in a committed relationship, she only has one male sex partner, but she does not know his HIV status and is uncertain about her partner’s fidelity. During previous appointments, you have discussed HIV risk with her and encouraged her to ask her partner to use condoms. However, she is not always able to convince him to use them, and reports having unprotected sex with her partner.
HIV antigen/antibody and RNA lab tests confirm that she is HIV-negative, though she has previously been treated for STDs. Her medical history is otherwise unremarkable.
In general, how much of a concern is each of the following to you in prescribing PrEP?
|
Not at all a concern |
A slight concern |
Somewhat a concern |
A moderate concern |
A major concern |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
In general, how much of a concern is each of the following to you in prescribing PrEP?
|
Not at all a concern |
A slight concern |
Somewhat a concern |
A moderate concern |
A major concern |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
In general, how much of a concern is each of the following to you in prescribing PrEP?
|
Not at all a concern |
A slight concern |
Somewhat a concern |
A moderate concern |
A major concern |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
[If # of responses rated somewhat/moderate/major concern > 3, carry forward only previous questions rated somewhat, a moderate, or a major concern]
What are your top 3 concerns about the use of PrEP as part of HIV prevention approaches? Please select up to 3 items.
Effectiveness of PrEP
Cost to patients
Your knowledge about PrEP
Staff time involved
Completing prior authorizations
Not certain who PrEP is right for
Frequency of follow-up visits for monitoring
Provider reimbursement for visits
Your comfort discussing sexual matters
Adherence challenges
Drug resistance
Risk compensation (i.e., decreased condom use)
Long-term/severe toxicity
Short-term side effects during product use
Other, specify: _____________
How much do you agree with the following statements?
|
Completely disagree |
Somewhat disagree |
Neither agree nor disagree |
Somewhat agree |
Completely agree |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
If an online tool were available to review PrEP data and prescribing guidelines, help screen for PrEP indications, and provide additional PrEP education and resources, how likely would you be to use it?
Very likely
Somewhat likely
Somewhat unlikely
Very unlikely
We would like to ask you more about injections.
When a patient wants to stop receiving PrEP injections, the patient may need to take oral PrEP pills daily for up to 1 year to protect against resistant HIV. This is because after the last injection, the PrEP medication slowly leaves the body, and at some point, the amount of medication remaining in the body is too little to protect against HIV, but is enough to put someone at risk of developing resistant HIV if they acquire infection. We are interested to know whether this affects your opinion about the injection.
How likely would you be to prescribe an injection every two months if it also meant that patients will be recommended to take daily oral PrEP pills for 1 year after stopping use of the injection?
Not at all likely
A little likely
Somewhat likely
Very likely
Extremely likely
Now, we have a few questions about you and your health care practice.
How long have you been practicing?
_____________ years
Do you see any of the following categories of patients? Please select all that apply
Men who have sex with men
Women
Transgender women or men
Adolescents
Injection drug users
Persons living with HIV
Persons without HIV who have a partner with HIV
U None of the above
[If seen any patients] Have you discussed oral PrEP with any of these patients? Please select all that apply
[carry forward responses from last question (except Persons living with HIV)]
Men who have sex with men
Women
Transgender women or men
Adolescents
Injection drug users
Persons without HIV who have a partner with HIV
Our last few questions are about your personal background.
What sex were you assigned at birth, on your original birth certificate?
Male
Female
I don’t know
Do you currently describe yourself as male, female, or transgender?
Male
Female
Transgender
None of these
Which of the following best represents how you think of yourself?
Lesbian or gay
Straight, that is, not lesbian or gay
Bisexual
Something else
I don’t know
What is your ethnicity?
Hispanic or Latino
Not Hispanic or Latino
How would you describe your race? Please select all that apply
American Indian or Alaska Native
Asian
Black or African American
Native Hawaiian or Other Pacific Islander
White
Thank you for taking the time to complete this survey. We truly value your opinions and the information you have provided.
If you are interested in learning more about prescribing PrEP, please visit https://www.cdc.gov/hiv/clinicians/prevention/prep.html
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| Author | Browne, Erica |
| File Modified | 0000-00-00 |
| File Created | 2022-10-18 |
© 2026 OMB.report | Privacy Policy