Supporting Statement 508
Supporting Statement 508.docx
Applications for Part C Medicare Advantage, 1876 Cost Plans, and Employer Group Waiver Plans to Provide Part C Benefits (CMS-10237)
OMB: 0938-0935
Supporting Statement Part A
Applications for Part C Medicare Advantage, 1876 Cost Plans, and Employer Group Waiver Plans to Provide Part C Benefits
CMS-10237, OMB 0938-0935
Note: The title of this information collection request is, “Medicare Advantage Application - Part C and 1876 Cost Plan Expansion Application Regulations under 42 CFR 422 (Subpart K) & 417.400.” In this iteration we are revising the title to read, “Applications for Part C Medicare Advantage, 1876 Cost Plans, and Employer Group Waiver Plans to Provide Part C Benefits.”
Background
The Balanced Budget Act of 1997 (BBA) Pub. L. 105-33, established “Part C” in the Medicare statute (sections 1851 through 1859 of the Social Security Act (the Act)) called Medicare+Choice. Under section 1851(a)(1) of the Act, every individual entitled to Medicare Part A and enrolled under Part B, except for most individuals with end-stage renal disease (ESRD), could elect to receive benefits either through the Original Medicare Program or an Medicare+Choice plan, if one was offered where he or she lived.
The Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA) Pub. L. 108-173 established the Medicare Prescription Drug Benefit Program (Part D) and made revisions to the provisions of Medicare Part C, governing what is now called the Medicare Advantage (MA) program (formerly Medicare+Choice). The MMA directed that important aspects of the new Medicare Prescription Drug Benefit Program under Part D be similar to and coordinated with regulations for the MA program. The MMA changes made managed care more accessible, efficient, and attractive to beneficiaries seeking options to meet their needs.
The final rules for the MA and Part D prescription drug programs appeared in the Federal Register on January 28, 2005 (70 FR 4588 through 4741 and 70 FR 4194 through 4585, respectively). Many of the provisions relating to applications, marketing, contracts and the new bidding process for the MA program became effective on March 22, 2005, 60 days after publication of the rule, so that the requirements for both programs could be implemented by January 1, 2006.
The MA program offers several kinds of plans and health care choices which include the following:
Coordinated Care Plans (CCPs) – A CCP is an MA plan that offers health care through an established provider network that is approved by the Centers for Medicare and Medicaid Services (CMS). There are several types of plans that are considered CCPs, including:
Health Maintenance Organizations (HMO)
Local Preferred Provider Organizations (LPPOs)
Regional Preferred Provider Organizations (RPPOs)
Special Needs Plans (SNPs)
Medical Savings Account (MSAs) – An MSA plan is a type of MA plan that combines a high-deductible health plan with a medical savings account.
Private Fee-For-Service (PFFS) Plans – A Medicare PFFS plan is a type of MA plan that may or may not have a network of providers. Members of a PFFS plan may see any provider who is eligible to receive payment from Medicare and agrees to accept the PFFS’s terms and conditions of payment.
Section 1876 Cost Plan – A cost contract plan is paid based on the reasonable costs incurred by delivering Medicare-covered services to plan members. Enrollees in these plans may use the cost plan's network of providers or receive their health care services through Original Medicare. CMS no longer accepts new, initial Cost Plan applications. However, an existing/approved Cost Plan can submit a service area expansion (SAE) application to expand its service area.
Employer Group Waiver Plans (EGWPs) – The MMA provides employers and unions with a number of options for providing coverage to their Medicare – eligible members. The EGWPs can offer various health plan types such PFFS, CCPs, MSAs and RPPOs.
Applications for each of the plan types described above are included in this information collection.
This information collection includes the process for organizations wishing to provide healthcare services under MA plans. These organizations must complete an application annually (if required), file a bid, and receive final approval from CMS. The MA application process has two options for applicants that include (1) request for new MA product or (2) request for expanding the service area of an existing product. CMS utilizes the application process as the means to review, assess and determine if applicants are compliant with the current requirements for participation in the MA program and to make a decision related to contract award. This collection process is the only mechanism for organizations to complete the required MA application process.
Note: Organizations that wish to offer both Part C and Part D must complete a separate Part D application. CMS refers to these applicants as MA-PD applicants The Part D information collection is included under OMB control number 0938-0936 (CMS-10137).
A Justification
Need and Legal Basis
This clearance request is for the vital information collection process to ensure Part C applicants are in compliance with CMS requirements and the collection of data necessary to support the decision related to contract awards. As noted above, organizations wishing to
provide healthcare services under MA plans must complete an application, file a bid, and receive final approval from CMS.
Collection of this information is mandated by the Code of Federal Regulations, MMA, and CMS regulations at 42 CFR 422, subpart K, in “Application Procedures and Contracts for Medicare Advantage Organizations.” In addition, the Medicare Improvement for Patients and Providers Act of 2008 (MIPPA) further amended titles XVII and XIX of the Social Security Act.
Information Users
CMS will collect and review information under the solicitation of Part C applications for the various health plan product types described in the Background section above. CMS will use the information to determine whether the applicants meet the requirements to become an MA organization and are qualified to provide a particular type of MA plan. The application consists of attestations and uploads that help CMS determine that the organization:
Is licensed by the State (see 42 CFR 422.501(c)(1) and 422.503(b)(2);
Has the management, financial, and operational capabilities to operate an MA contract (see 42 CFR 422.503(b)(4):
Demonstrates acceptable past performance history (see 42 CFR 422.502(b); and 4. Meets the minimum enrollment requirements to offer an MA plan (see 1857(b) and 42 CFR 422.503(b)(3).
The application process is open to all health plans that want to participate in the MA program. The application is distinct and separate from the bid process, and CMS issues a determination on the application prior to bid submissions, or before the first Monday in June.
Information Technology
In the application process, technology is used in the collection, processing and storage of the data. Specifically, applicants must submit the entire application and supporting documentation through CMS’ Health Plan Management System (HPMS). This is the case for both the MA initial and SAE applications.
The MA application has several sections that require the applicants to respond to attestations based upon the application type (new MA product or expanding services area for existing MA product) and health plan type (e.g., CCP, MSA, etc.). For example, when an applicant accesses HPMS to complete the application process for a new/initial MA product, the applicant would be guided through the parts of the application that need to be completed for initial applicants. Initial applicants have additional attestations than entities that currently hold contracts with CMS, such as the requirement to complete the two experience and organization history attestations.
Additionally, the application has documents referred to as “templates” which are forms that need to be downloaded from HPMS, completed by the applicant, and uploaded into HPMS.
Duplication of Similar Information
The MA application that is accessed via HPMS contains information essential for the operation and implementation of the MA program. It is the only standardized mechanism available to record data from organizations interested in contracting with CMS to offer an MA plan. Where possible, we have modified the standard application to auto-populate information that is captured in prior data collection and resides in HPMS. Otherwise, the form does not duplicate any information currently collected.
Small Business
The collection of information will have a minimal impact on small businesses since applicants must possess an insurance license and be able to accept substantial financial risk. Generally, state statutory licensure requirements effectively preclude small businesses from being licensed to bear risk needed to serve Medicare enrollees.
Less Frequent Collection
This is an annual collection. If this information were collected less frequently, CMS will have no mechanism to allow new applicants an opportunity to demonstrate that applicants meet the CMS requirements and support determination of contract awards or denials.
Special Circumstances
Each applicant is required to enter and maintain data in the HPMS. Prompt entry and ongoing maintenance of the data in HPMS will facilitate the tracing of the applicant’s application throughout the review process. If the applicant is awarded a contract after negotiation, the collection of information will be used for frequent communications during implementation of the MA organization’s program. Applicants are expected to ensure the accuracy of the collected information on an ongoing basis.
Federal Register Notice/Outside Consultation Federal Register Notices & Comments
60 Day Notice: Volume:
84 Page number: 48145
Number of Comments :
7 Publication
date:
09/12/2019 Responses to the comments can be
located on the Comment Tracker.
Payment/Gift to Respondent
While there are no gifts associated with this collection, the application is required to receive a government contract.
Confidentiality
Consistent with federal government and CMS policies, CMS will protect the confidentiality of the requested proprietary information. Specifically, only information within a submitted application (or attachments thereto) that constitutes a trade secret, privileged or confidential information, (as such terms are interpreted under the Freedom of Information Act and applicable case law), and is clearly labeled as such by the applicant, and which includes an explanation of how it meets one of the expectations specified n 45 CFR Part 5, will be protected from release by CMS under 5 U.S.C. §552(b)(4). Information not labeled as trade secret, privileged, confidential or does not include an explanation of why it meets one or more of the Freedom of Information Act exceptions in 45 CFR Part 5 will not be withheld from release under 5 U.S. C. §552(b)(4).
Sensitive Questions
Other than the labeled information noted above in section 10, there are no sensitive questions included in the information request.
Wages
To derive average costs, we used data from the U.S. Bureau of Labor Statistics’ (BLS) May 2018 National Occupational Employment and Wage Estimates for all salary estimates (http://www.bls.gov/oes/current/oes_nat.htm). We selected the position of Compliance Officer because this position is a key contact identified by MA plans. CMS typically interacts with the Compliance Officer in matters related to the Part C/MA application after it is submitted to CMS. In this regard, the following table presents the mean hourly wage, the cost of fringe benefits (calculated at 100 percent of salary), and the adjusted hourly wage.
Table 1 – BLS Labor Rate
-
Occupation Title
Occupation Code
Mean Hourly Wage ($/hr)
Fringe Benefit ($/hr)
Adjusted Hourly Wage ($/hr)
Compliance Officers
13-1041
34.86
34.86
69.72
As indicated, we are adjusting our employee hourly wage estimates by a factor of 100 percent. This is necessarily a rough adjustment, both because (1) fringe benefits and overhead costs vary significantly from employer to employer, and (2) because methods of estimating these costs vary widely from study to study. Nonetheless, there is no practical alternative, and we believe that doubling the hourly wage to estimate total cost is a reasonably accurate estimation method.
Requirements and Associated Burden Estimates
Organizations wishing to provide healthcare services under Part C/MA plans must complete an application, file a bid, and receive final approval from CMS. Existing Part C/MA plans may request to expand their contracted service area by completing the SAE application.
This clearance request is for information collection of the health plan types described in the Background section of this document. The application process is open to all health plans that want to participate in the Part C/MA program.
Time by Application Type
In total, for CY 2021 CMS estimates that it will receive 435 applications. This would amount to 6,754 total annual hours. The estimated burden hours are based on an internal assessment of application materials that are required for submission by the applicants. The application process has two options for applicants that include (1) request for new MA product, or (2) request for expanding the service area of an existing product. If an applicant is applying for a new MA product then the application process would be longer because the required completion of attestations and potential templates that need to be completed will require more effort than an applicant that is requesting to expand their service area via the SAE application.
The chart below describes types of MA product types (as described in the Background section) that can submit applications. The chart is identifying application options in terms of initial applications and SAE applications (NOTE: No new 1876 Cost Plans can submit new applications).
Table 2 – Summary of Annual Burden Hours
Application/ Responses |
Initial (CCP, PFFS- Network, MSA- Network, EGWP ) |
SNP Initial |
PFFS (Initial- Non- network) |
MSA (Initial Non- Network) |
SAE (CCP, PFFS- Network , MSA- Network EGWP) |
SNP SAE |
PFFS (SAE- Non- network) |
MSA (SAE Non- Network) |
Direct EGWP |
Cost Plan SAE |
Summary |
Expected Applications/ Responses |
70 |
85 |
0 |
1 |
185 |
91 |
2 |
0 |
0 |
1 |
435 |
Review Instructions (#of hours) |
1.0 |
1.0 |
1.0* |
1 |
0.5 |
0.5 |
.5 |
.5* |
0.5* |
0.5 |
5 |
Complete Application / Proposal (# of hours) |
32.0 |
9.0 |
32.0* |
32.0 |
15.0 |
6.5 |
18.5 |
21* |
0.5* |
17.5 |
132 |
Estimated # of hours per application /proposal |
33 |
10 |
33* |
33 |
15.5 |
7 |
19 |
21.5* |
1* |
18 |
137 |
Annual Burden hours |
2,310 |
850 |
0 |
33 |
2,868 |
637 |
38 |
0 |
0 |
18 |
6,754 |
*Numbers not included in Summary column given expected workload of 0.
Cost by Application Type
The estimated wage burden for the MA Part C Application is $470,870 based on an estimate wage rate of $69.72/hr wage. The median cost per application is $1,253 (18 hours * $69.72=
$1,253).
Table 3 – Summary of Industry Wage Burden
Application/ Responses |
Initial (CCP, PFFSNetwork, MSA- Network EGWP ) |
SNP Initial |
PFFS (Initial- Non- network) |
MSA (Initial) |
SAE (CCP, PFFS- Network, MSA- Network EGWP) |
SNP SAE |
PFFS (SAE - Non- network) |
MSA (SAE Non- Network) |
Direct EGWP |
Cost Plan SAE |
Total |
Annual burden Hours |
2,310 |
850 |
0 |
33 |
2,868 |
637 |
38 |
0 |
0 |
18 |
6,754 |
Per Hour Wages |
$69.72 |
$69.72 |
$69.72 |
$69.72 |
$69.72 |
$69.72 |
$69.72 |
$69.72 |
$69.72 |
$69.72 |
$69.72 |
Total Wage burden |
$161,035 |
$59,262 |
$0 |
$2,300 |
$199,957 |
$44,412 |
$2,649 |
$0 |
$0 |
$1,255 |
$470,870 |
Information Collection Attachments
Part C -Medicare Advantage and 1876 Cost Plan Expansion Application
Part C -Medicare Advantage and 1876 Cost Plan Expansion Application is submitted electronically via HPMS. CMS provides the paper version of the application in the annual Part C PRA package. The table of contents identifies the key components of the application, which are also summarized below.
General Information – This section provides overview of the MA program, description of MA product types, description of HPMS, key due dates related to the application process;
Instructions – This section provides general information on how to complete the application process , specific instructions related to certain health plan product types such as EGWPs, SNPs and Cost Plans, and a chart is provided that summarizes the various attestations that are required to be completed by the applicant based upon heath plan type;
Attestations – This section has all the attestations that are utilized in the application process by both new MA product applicants and SAE applicants. The required attestations for a new MA product applicant is greater than the number of attestations required for an SAE applicant (See chart below);
Document Upload Templates – This section has all the required templates that an applicant may need to complete based upon the type of application and /or health plan type. Currently there are 10 upload documents in this area of the application;
Appendix 1- Solicitations for Special Needs Plan (SNP) Application – This section includes the application for applicants that want to offer a SNP. This section would be completed to reflect the type of SNP and population of beneficiaries the applicant wants to serve. Note this section also has some specific attestations and template upload documents that are required for SNP applicants;
Appendix II- Employer/union – Only Group Waiver Plans (EGWPs) MAO “800” Series – this section is specific to EGWP applicants only. As noted above for the SNP section this section also has attestations and/or upload documents that are specific to this application type.
Appendix III- Employer/Union Direct Contract for MA – This section has specific requirements for this health plan type that the applicant is required to complete.
Appendix IV-Medicare Cost Plan Service Area Expansion Application – This section is required for any existing Cost Plan that wants to request an expansion in their service area. Note: no new application for Cost Plans can be submitted to CMS.
HPMS is the primary information collection vehicle through which organizations will communicate with CMS during the application process, bid submission process, ongoing operations of the MA program or Medicare Cost Plan contracts, and reporting and oversight activities.
Table 4 - Chart of Required Attestations by Application Type (non-SNP)
Attestation Section Name |
Section # |
Initial Applicants |
|
Service Area Expansion |
|||||||
|
|
CCP |
PFFS |
RPPO |
MSA |
|
CCP |
PFFS |
RPPO |
MSA |
COST |
Management, Experience, and History |
3.1 |
X |
X |
X |
X |
|
|
|
|
|
|
Administrative Management |
3.2 |
X |
X |
X |
X |
|
X |
X |
X |
X |
X |
State Licensure |
3.3 |
X |
X |
X |
X |
|
X |
X |
X |
X |
X |
Program Integrity |
3.4 |
X |
X |
X |
X |
|
|
|
|
|
|
Compliance Plan |
3.5 |
X |
X |
X |
X |
|
|
|
|
|
|
Key Management Staff |
3.6 |
X |
X |
X |
X |
|
|
|
|
|
|
Fiscal Soundness |
3.7 |
X |
X |
X |
X |
|
X |
X |
X |
X |
|
Service Area |
3.8 |
X |
X* |
X |
X* |
X |
X* |
X |
X* |
X |
|
CMS Provider Participation Contracts & Agreements |
3.9 |
X |
X |
X |
X |
|
X |
X |
X |
X |
X |
Contracts for Administrative & Management Services |
3.10 |
X |
X |
X |
X |
|
X |
X |
X |
X |
X |
Quality Improvement Program |
3.11 |
X |
X |
X |
X |
|
|
|
|
|
|
Marketing |
3.12 |
X |
X |
X |
X |
|
|
|
|
|
|
Eligibility, Enrollment, and Disenrollment, |
3.13 |
X |
X |
X |
X |
|
|
|
|
|
|
Working Aged Membership |
3.14 |
X |
X |
X |
X |
|
|
|
|
|
|
Claims |
3.15 |
X |
X |
X |
X |
|
|
|
|
|
|
Communication between MAO and CMS |
3.16 |
X |
X |
X |
X |
|
|
|
|
|
|
Grievances |
3.17 |
X |
X |
X |
X |
|
|
|
|
|
|
Organization Determination and Appeals |
3.18 |
X |
X |
X |
X |
|
|
|
|
|
|
Health Insurance Portability and Accountability Act of 1996 (HIPAA) |
3.19 |
X |
X |
X |
X |
|
|
|
|
|
|
Continuation Area |
3.20 |
X |
X |
X |
X |
|
X |
X |
X |
X |
|
Part C Application Certification |
3.21 |
X |
X |
X |
X |
|
X |
X |
X |
X |
X |
Access to Services |
3.22 |
|
X |
|
|
|
|
X |
|
|
|
Claims Processing |
3.23 |
|
X |
|
X |
|
X |
|
X |
|
|
Payment Provisions |
3.24 |
|
X |
|
X |
|
X |
|
X |
|
|
General Administration/ Management |
3.25 |
|
|
|
X |
|
|
|
X |
|
|
|
|||||||||||
Past Performance |
3.26 |
X |
X |
X |
X |
|
X |
X |
X |
X |
X |
*Applies to network PFFS and MSA applicants.
Capital Cost (Maintenance of Capital Costs)
We do not anticipate additional capital costs. CMS requirements do not require the acquisition of new systems or the development of new technology to complete the application.
System requirements for submitting HPMS applicant information are minimal. MAOs will need the following access to HPMS: (1) Internet or Medicare Data Communications Network (MDCN) connectivity, (2) use of Microsoft Internet Explorer web browser (version 5.1 or higher) with 128-bits encryption and (3) a CMS-issued user ID and password with access rights to HPMS for each user within the MAO’s organization who will require such access. CMS anticipates that all qualified applicants meet these system requirements and will not incur additional capital costs.
Cost to Federal Government
To derive average costs, we used data from the Office of Personnel Management’s (OPM) 2018 Salary Table for the Washington-Baltimore-Northern Virginia locality (https://www.opm.gov/policy-data-oversight/pay-leave/salaries-wages/salary- tables/18Tables/html/DCB_h.aspx). The following table presents the hourly wage, the cost of fringe benefits (calculated at 100 percent of salary), and the adjusted hourly wage. Table 5 – Occupation-Specific OPM Labor Rates
-
Occupation
Grade/Step
Wage ($/hr)
Fringe Benefit ($/hr)
Adjusted Hourly Wage ($/hr)
Regional Office Account Managers/ Central Office Health Insurance Specialist
13/5
52.66
52.66
105.32
Regional Office Supervisor
14/5
62.23
62.33
124.66
As indicated, we are adjusting our employee hourly wage estimates by a factor of 100 percent. This is necessarily a rough adjustment, both because (1) fringe benefits and overhead costs vary significantly from employer to employer, and (2) because methods of estimating these costs vary widely from study to study. Nonetheless, there is no practical alternative and we believe that doubling the hourly wage to estimate total cost is a reasonably accurate estimation method.
Our estimated cost is based on the budgeted amount for application review and estimate wages of key reviewers and support staff. Note the Part C applications are submitted by various MA plans across the country.
The primary review of the Part C applications is the responsibility of Regional Office staff which is usually at the GS 13 level with position type such as RO Account Managers. In addition, the Central Office staff (primarily in the Medicare Drug & Health Plan Contract Administration Group (MCAG) is also required to perform some portions of the Part C application review process which is usually of the GS 13 grade level and position type such as Health Insurance Specialist.
Regional Office Supervisor is requested to confirm the RO staff review decisions. The RO Supervisor is usually at the GS14 grade level.
Table 6 - Annualized Cost to Federal Government
-
CMS Staff
Hour per Application
Application Volume
Total Hours
Hourly Rate
Projected Costs
Cost per Application
HPMS
Systems staff
4
435
1740
$105.32
$183,257
$421
Central Office Health Insurance Specialist
4
435
1740
$105.32
$183,257
$421
Regional Office Account Manager
10
435
4350
$105.32
$458,142
$1,053
Regional Office Supervisor
4
435
1740
$124.66
$216,908
$499
Total
22
-
9,570
-
$1,041,564
$2,394
Program or Burden Changes
There are minor changes to the burden estimates for CY 2021 when compared to CY 2020 (and prior years). These changes are:
Changes in labor rates
Added attestation
Table 7 provides a summary comparison burden estimates between CY 2020 and CY 2021.
Table 7 - Summary of Burden Hours Comparison CY2020 to CY2021
-
CY2020
Number of Respondents
CY 2020
Estimates (hours)
CY2020
Annual Burden Hours
CY2021
Number of Respondents
CY 2021
Estimates (hours)
CY2021
Annual Burden Hours
Initial (CCP,PFFS-
Network, MSA,- Network, EGWP )
60
33
1,980
70
33
1,980
SNP Initial
80
10
800
85
10
800
PFFS non- Network (initials)
0
33
0
0
33
0
MSA non- Network (initials)
1
33
33
1
33
33
SAE (CCP,PFFS-
Network, MSA,- Network, EGWP )
170
15.5
2,635
185
15.5
2,635
SNP SAE
86
7
602
91
7
602
SNP Renewal Only
0
0
0
0
0
0
PFFS (SAE-
Non- network)
2
19
38
2
19
38
MSA (SAE-
Non- network)
0
21.5
0
0
21.5
0
Direct EGWP
0
1
0
0
1
0
Cost Plan SAE
1
18
18
1
18
18
Total
400
191
6,106
435
191
6,754
Table 8 below provides additional detail regarding the changes in hours between the CY 2020 and CY 2021 applications. The narrative explanation for the reduction in burden for the attestations and uploads is provided in section 15.3 through 15.5 below. Table 8: Changes in Burden Across Attestations and Uploads
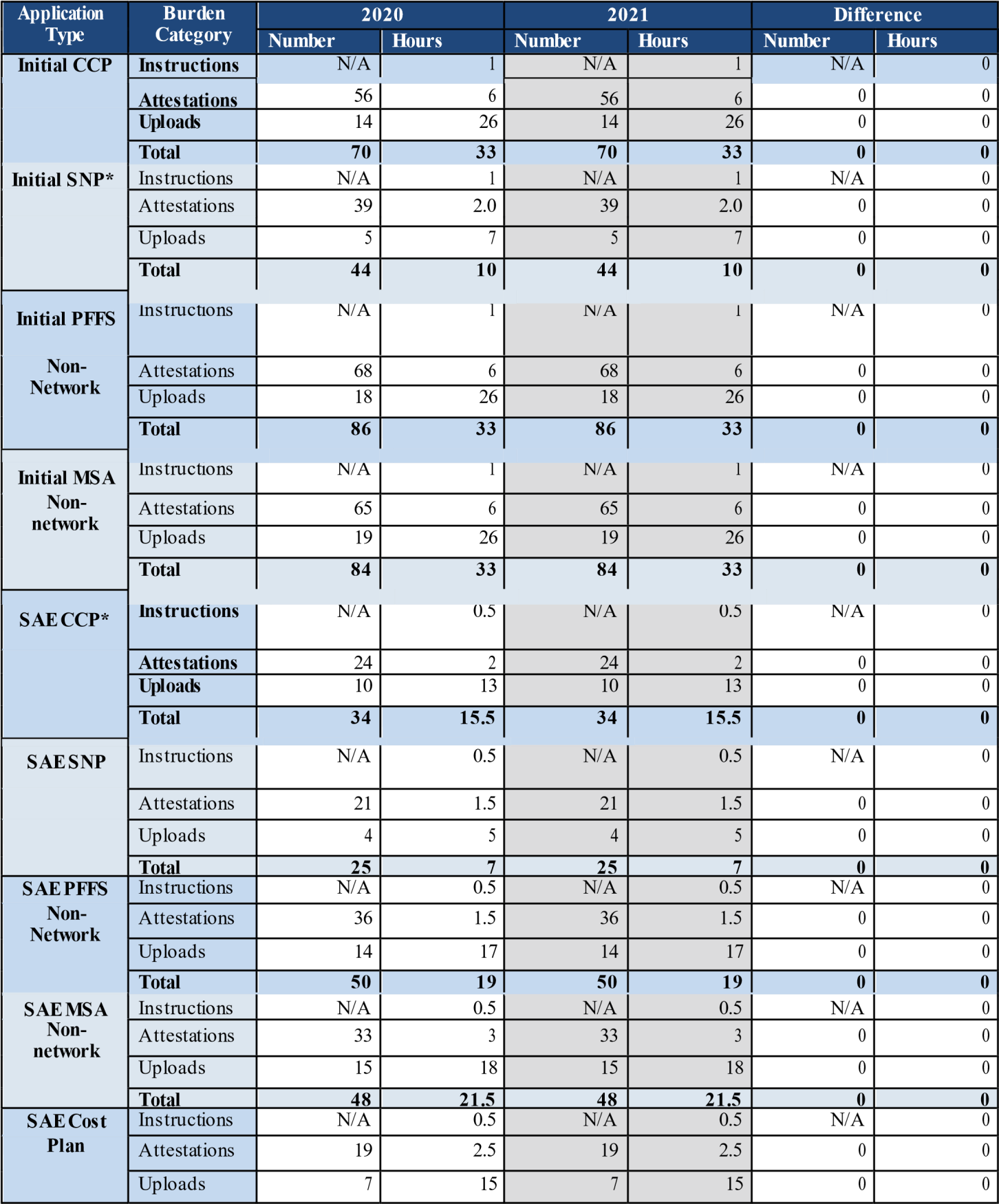
|
Total |
26 |
18 |
26 |
18 |
0 |
0 |
*SNP application attestations and uploads vary slightly by application type. |
|||||||
In addition to changes to CMS’s burden estimate for industry, we estimate significant Government burden estimates will remain constant, which are shown in the table below.
Table 9 - Summary of Government Burden Changes: Hours Per Application
-
CMS Staff
CY 2020
Hours
CY 2021
Hours
Difference
HPMS Systems staff
4
4
0
Central Office Health Insurance
Specialist
4
4
0
Regional Office Account Manager
10
10
0
Regional Office Specialist HSD Review
0
0
0
Regional Office Supervisor
4
4
0
SNP Clinical
0
0
0
Total
22
22
0
The sections below provide additional detail to support the changes described above.
Burden Changes Driven by Workload Volumes
For the CY 2020 application cycle, CMS had an approximate 20% increase in MA SAE applications. We believe this increase corresponds with the implementation of the triennial review. CMS also had an approximate increase of 11% in MA initial applications. We believe that this increase was also due to increased industry preparedness. Based on comparing the CY 2021 data to CYs 2015-2020, the CY 2021 volumes align with historic trends.
Similar to CY 2020 MA application volumes, CMS had an increase in SNP applications in CY 2020 as compared to CY 2019. CMS noted an approximate 62% increase in the number of SNP initial applications submitted in CY 2020 when compared to CY 2019, and an increase of 3% SNP SAE applications. Organizations seeking SNP applications must first be qualified in the respective SNP service area through the MA application process. Therefore, initial SNP applications often have corresponding initial MA applications. CMS also sees MA SAE applications submitted when a SNP wants to expand their service area to offer services in a new state or county.
Given the fluctuations between CY 2019and 2020, CMS estimated the CY 2021 application workloads in Table 9 below by analyzing application receipt data from CYs 2014-2019. CMS calculated the CY 2021 workload by taking the median across these years, but excluded CY 2014 as an outlier since the initial workload volumes were significantly higher than any other year.
Table 10 - Workload Comparison: CY 2020 and CY 2021
Application/ Responses |
Initial (CCP, PFFS- Network, MSA- Network EGWP ) |
Initial with SNP |
PFFS (Initial- Non- network) |
MSA (Initial Non- Network) |
SAE (CCP, PFFS- Network, MSA- Network, EGWP) |
SAE with SNP |
PFFS (SAE- Non- network) |
MSA (SAE Non- Networ k |
Direct EGWP |
Cost Plan SAE |
Summary |
CY 2020 Expected Applications/ Responses |
60 |
80 |
0 |
1 |
170 |
86 |
2 |
0 |
0 |
1 |
400 |
CY 2021 Expected Applications/ Responses |
70 |
85 |
0 |
1 |
185 |
91 |
2 |
0 |
0 |
1 |
435 |
Difference |
+10 |
+5 |
0 |
0 |
+15 |
+5 |
0 |
0 |
0 |
0 |
+35 |
Burden Changes Drive by Labor Rate Adjustments
For industry burden, we have adjusted our cost estimates by using the most recent BLS wage data, as discussed in section 12.1 above. Similarly, for CMS burden, we have adjusted our cost estimates by using the most recent labor rate calculated by OPM, as discussed in section 14 above.
Table 11 - Labor Rate Comparison: CY 2020 and CY 2021
-
CY 2020
CY 2021
Difference
BLS Hourly Rate
$68.78
$69.72
+$.94
OMB Hourly Rate – GS-13
$105.32
$105.32
+0.00
OMB Hourly Rate – GS-14
$124.66
$124.66
+0.00
Changes Driven by Comments
CMS made several changes that were driven by the comments received during the 60 Day PRA collection. CMS updated the dates in the Administrative Management and Two year Prohibition section of the application to reflect the correct two year period prior to the expected January 1, 2021 effective date of the contract. The eligibility, enrollment and disenrollment section was also modified to reflect the recent announcement that CMS will be changing the timeframe for plan sponsor submission of enrollment and payment certifications from monthly to quarterly. Appendix I of the SNP application was also updated to clarify some of the instructions within the section to provide further clarity to the applicants. The language was also modified in the D-SNP State Medicaid Agency Contract matrix to match the updated regulation.
Publication and Tabulation Dates
This information is not published or tabulated.
Expiration Date
CMS is not requesting an exemption from displaying the expiration date. Note this collection request is submitted annually for the Part C application.
Certification Statement
There are no exceptions to the certification statement.
B. Collection of Information Employing Statistical Methods
There has been no statistical method employed in this collection.
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| File Title | Supporting Statement for Applications for |
| Author | CMS |
| File Modified | 0000-00-00 |
| File Created | 2021-01-14 |
© 2026 OMB.report | Privacy Policy