Form 0920-19MM EHR data collection tool
The Centers for Disease Control and Prevention (CDC) Study on Disparities in Distress Screening among Lung and Ovarian Cancer Survivors
Att 4- EHR data collection tool DS
EHR Data
OMB: 0920-1270
Attachment 4: EHR data collection tool and instructions
Public reporting burden for this collection of information is estimated to average 7.5 hours per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing the collection of information. An agency may not conduct or sponsor, and a person is not required to respond to, a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing this burden to: CDC, XXXX Branch, ADDRESS, CITY, STATE ZIP, ATTN: PRA (XXXX-XXXX). Do not return the completed form to this address.
EHR Abstraction Tool for Distress Screening and Outcome Data
Elements
Notes:
The MS Access tool is designed to accommodate a one to many (1:m) relationship between the patient’s first screen and the assessments and interventions, respectively, where one patient case may be linked to one distress screening but multiple assessments and multiple interventions based on the single distress screening.
The data can be queried and exported at any of the three levels (patient, screening, intervention). For instance, intervention-level data may be reshaped so that each row represents one patient in the exported database.
Screenshot of MS Access introductory screen with burden statement:

Screenshot of MS Access introductory screen with burden statement:

Screenshot of MS Access data entry for distress screening:
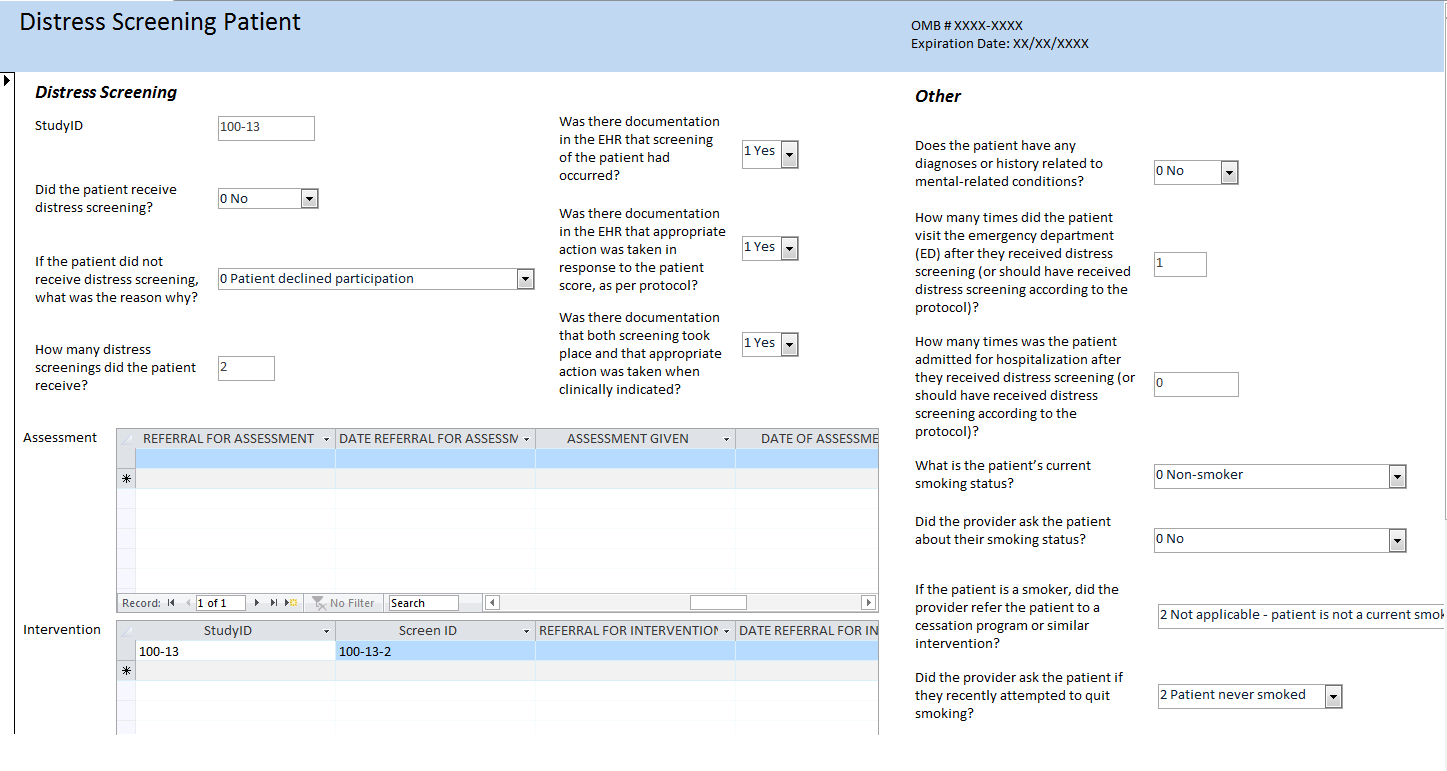
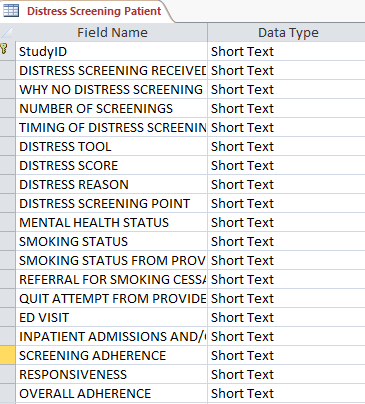
Screenshot of Patient-level table:
Screenshot of Assessment-level table:

Screenshot of Intervention-level table:

Instructions for healthcare facility IT department to extract data from EHR
The Centers for Disease Control and Prevention (CDC) is sponsoring a study to examine the distress screening procedures among ovarian and lung cancer patients at cancer treatment facilities and programs across the country. Westat, a research organization located in Maryland, is working with the CDC on data collection for the study.
For this study, we are requesting an extraction of specific data items from your healthcare facility’s EHR system. We understand that your healthcare facility may have discrete fields that use specific code systems or standardized formats for data items in your EHR system, while you may collect other data in less standardized ways. Therefore, we are requesting an extract of demographic and cancer-related data items that EHR systems are likely to capture in a more standardized manner. For other data items that EHR systems are not as likely to capture in specific data fields but may capture in other ways such as in a notes section or as a scanned document, we will work with your healthcare facility to choose an ideal method for abstracting this data from the EHR. The following document will focus on the extraction of more standardized data items.
Follow the instruction below to identify the cases that you should select for the study, to create a report with the extract of data items of interest, and to submit the report to Westat.
I. Selection Criteria
Select cancer cases that meet the following criteria:
Ovarian cancer cases with ICD-9-CM diagnosis code 183.0 or ICD-10-CM diagnosis code C56.-
Lung cancer cases with ICD-9-CM diagnosis codes 162.2, 162.3, 162.4, 162.5, 162.8, 162.9 or ICD-10-CM diagnosis codes C34.0-, C34.1-, C34.2, C34.3-, C34.8-, C34.9-
Of the cancer cases selected above, only select those cases where the date of the first encounter related to the cancer diagnosis (using the associated diagnosis codes above) occurred in 2016 or 2017
Provide the number of cases to study staff. If the number of cases is large, they will work with you to randomly select a subset of cases.
II. Data items to extract for report
We are requesting an extract of specific data items in a standardized format, as defined in the table below. However, if your EHR uses a different code set for a data item and you are unable to translate your data to fit the code set we specified, please let study staff know.
Create a report that includes the following data elements and code them or format them as defined below. You only need to include the code and not the label associated with the code (for example, for the data item “Sex”, please code “1” and not “1 Male”. Please create the report in a delimited or fixed-width format such as .csv, .xls, or .xlsx.
Data Element |
Description |
Choice List (if applicable) or Format |
Calculation (if applicable) |
Source and other notes |
RACE |
The patient's race |
0 White 1 Black or African American 2 Asian 3 Native Hawaiian or Other Pacific Islander 4 American Indian or Alaska Native 5 Other Race |
|
Race & Ethnicity – CDC (https://phinvads.cdc.gov/vads/ViewValueSet.action?id=67D34BBC-617F-DD11-B38D-00188B398520) |
SPANISH/HISPANIC ORIGIN |
Whether the patient is of Spanish/Hispanic origin |
0 Not Hispanic or Latino 1 Hispanic or Latino |
|
Race & Ethnicity – CDC (https://phinvads.cdc.gov/vads/ViewValueSet.action?id=35D34BBC-617F-DD11-B38D-00188B398520) |
SEX |
The sex of the patient |
1
Male 5
Genderqueer, neither exclusively male nor female |
|
SNOMED CT (https://www.healthit.gov/isa/representing-patient-gender-identity) |
AGE AT DIAGNOSIS |
The age of the patient at the time of the diagnosis for the specific tumor of interest |
Number format |
Use the patient’s birthdate and subtract it from the patient’s date of diagnosis to determine the patient’s age at diagnosis |
|
CURRENT AGE |
The age of the patient at the time that the data was extracted/abstracted from the facility |
Number format |
Use the patient’s birthdate and subtract it from the current date to determine the patient’s age at diagnosis |
|
POSTAL/ZIP CODE |
The postal/zip code of the patient at the time of diagnosis |
Five-digit postal/zip code |
|
|
PAYMENT SOURCE |
The source of payment used during time of diagnosis/treatment at the healthcare facility |
1 Medicare 2 Medicaid 3 Other Government (Federal/State/Local) 4 Departments of Corrections 5 Private Health Insurance 6 Blue Cross/Blue Shield 7 Managed Care, Unspecified 8 No payment from an organization/agency/program/private payer listed 9 Miscellaneous/other |
|
Source of Payment Typology (PHDSC) |
DATE OF DIAGNOSIS |
The date that the tumor was diagnosed, whether through clinical means (such as physical exam or imaging), biopsy or other microscopic methods |
YYYYMMDD |
|
|
DATE OF FIRST CANCER ENCOUNTER |
The date of the patient’s first encounter at the facility where cancer is the primary diagnosis/reason for the encounter |
YYYYMMDD |
|
Use the date of the patient’s earliest encounter where the primary diagnosis/reason for the encounter was coded using the ICD-9-CM or ICD-10-CM code associated with ovarian or lung cancer |
PRIMARY SITE |
The primary site (organ or location) that the cancer originated from |
Ovary ICD-9-CM: 183.0 ICD-10-CM: C56.-
Lung ICD-9-CM: 162.2, 162.3, 162.4, 162.5, 162.8, 162.9 ICD-10-CM: C34.0-, C34.1-, C34.2, C34.3-, C34.8-, C34.9- |
|
ICD-9-CM (applicable for claims on or before September 30, 2015), ICD-10-CM (applicable for claims on or after October 1, 2017)
NOTE: ICD-9 and ICD-10 codes only provide topography, not histology/morphology |
CANCER STAGE CLINICAL |
The stage of the cancer according to the AJCC TNM staging schema; staging schemas differ by primary site and are assigned by the physician; Clinical stage is typically assigned based on the evidence available before treatment |
Ovary I
Stage 1 Not Otherwise Specified (NOS) (localized)
Lung 0
Stage 0 (in situ) |
|
AJCC TNM Staging;
NOTE: Small cell lung cancer is sometime staged as either limited or extensive. Beginning with AJCC TNM 7th edition, small cell and non-small cell lung cancer were able to be staged using the same schema. |
CANCER STAGE PATHOLOGIC |
The stage of the cancer according to the AJCC TNM staging schema; staging schemas differ by primary site and are assigned by the physician; pathologic stage is assigned using the evidence available before treatment, in addition to additional evidence during and after surgery |
Ovary I
Stage 1 Not Otherwise Specified (NOS) (localized)
Lung 0
Stage 0 (in situ) |
|
AJCC TNM Staging
NOTE: Small cell lung cancer is sometime staged as either limited or extensive. Beginning with AJCC TNM 7th edition, small cell and non-small cell lung cancer were able to be staged using the same schema. |
III. Submitting data through Secure File Transfer Protocol (SFTP)
Please follow the steps outlined below to submit your data extract report through Westat’s SFTP.
Name the file:
We will provide you with a two-digit healthcare facility code that you will use to name your file
Use the naming convention [Two digit healthcare facility code]_Distress_EHR
Example: 11_Distress_EHR
Submit the file:
Upload the file to Westat’s Secure File Transfer Protocol website: https://securetransfer2.westat.com/
We will provide you with the username and password associated with the account that you will use to upload, as well as the name of the folder that you will upload the file to
After logging in to the site (and resetting your password, if you have not done so already), click on “Folders” on the panel to the left side of the screen
Navigate to the folder that was created for your specific healthcare facility (/Distribution/[HEALTHCARE FACILITY SPECIFIC FOLDER])
Click “Launch the Upload Wizard” and use the tool to choose the file for the report that you would like to upload and follow the prompts to upload the file
EHR Abstraction Data Entry Guide for Distress Screening and
Outcome Data Elements
Abstract data elements using available documentation in the patient’s EHR.
Question [Data element] |
Response Options |
What We’re Looking For |
GENERAL |
||
Study ID |
Two character/digit hospital code followed by three digit patient code (Ex: 01-001) |
Unique ID assigned by Westat to the patient solely for use in this study |
Date Case Entered |
Enter a date using the format MM/DD/YYYY |
Date case was abstracted into the abstraction tool |
Abstractor |
Initials of abstractor |
Enter your initials for cases that you abstract into the abstraction tool |
DEMOGRAPHICS AND CANCER |
||
[Race] |
0 White 1 Black or African American 2 Asian 3 Native Hawaiian or Other Pacific Islander 4 American Indian or Alaska Native 5 Other Race |
Code patient race; this may be standardly coded at the hospital level or may be available in a patient’s personal history |
[Spanish/Hispanic Origin] |
0 Not Hispanic or Latino 1 Hispanic or Latino |
Code patient Spanish/Hispanic origin; this may be standardly coded at the hospital level or may be available in a patient’s personal history |
[Sex] |
1 Male 2 Female 3 Female-to-Male (FTM)/Transgender Male 4 Male-to-Female (MTF)/Transgender Female 5 Genderqueer, neither exclusively male nor female 6 Other |
Code patient sex; this may be standardly coded at the hospital level or may be available in other documentation in EHR |
[Age at diagnosis] |
Enter a number |
Use the patient’s diagnosis date and birth date as documented in EHR and calculate the patient’s age based on the difference between the two dates (date of diagnosis – birth date) |
[Current age] |
Enter a number |
Use the current date (when extracting or abstracting EHR data) and the patient’s birth date as documented in EHR and calculate the patient’s current age based on the difference between the two dates. (current date – birth date) |
[Postal/zip code] |
Enter the five-digit postal/zip code |
Enter the patient’s five-digit postal/zip code |
[Payment source] |
1 Medicare 2 Medicaid 3 Other Government (Federal/State/Local) 4 Departments of Corrections 5 Private Health Insurance 6 Blue Cross/Blue Shield 7 Managed Care, Unspecified 8 No payment from an organization/agency/program/private payer listed 9 Miscellaneous/other |
Record the primary payment source for the patient’s care, if available |
[Date of diagnosis] |
Enter a date using the format MM/DD/YYYY |
Record the date of diagnosis for the relevant cancer; this is based on the date the tumor was diagnosed, whether through clinical means (such as a physical exam or imaging), biopsy, or other microscopic methods |
[Date of first cancer encounter] |
Enter a date using the format MM/DD/YYYY |
Record the date of the patient’s first encounter at the facility where cancer is the primary diagnosis/reason for the encounter, based on the ICD-9-CM or ICD-10-CM code |
[Primary site] |
1 Ovary 2 Lung |
Code whether the patient is an ovarian cancer case or a lung cancer case |
[Cancer stage clinical] |
Ovary I Stage 1 Not Otherwise Specified (NOS) (localized) IA Stage 1A (localized) IB Stage 1B (localized) IC Stage 1C (localized) II Stage 2 NOS (localized) IIA Stage 2A (localized) IIB Stage 2B (localized) IIC Stage 2C (localized) III Stage 3 NOS(localized) IIIA Stage 3A (localized) IIIB Stage 3B (localized) IIIC Stage 3C (localized) IV Stage 4 (metastasis)
Lung 0 Stage 0 (in situ) IA Stage 1A (localized) IB Stage 1B (localized) IIA Stage 2A (localized) IIB Stage 2B (localized) IIIA Stage 3A (localized) IIIB Stage 3B (localized) IV Stage 4 (metastasis) |
Record patient’s clinical cancer stage based on the AJCC TNM* staging schema; this may be documented in a staging form that the physician has completed, in a pathology report, etc.; note: cancer is staged clinically before the patient receives treatment
*American Joint Committee on Cancer – T (tumor) N (node) M (metastasis) |
[Cancer stage pathologic] |
Ovary I Stage 1 Not Otherwise Specified (NOS) (localized) IA Stage 1A (localized) IB Stage 1B (localized) IC Stage 1C (localized) II Stage 2 NOS (localized) IIA Stage 2A (localized) IIB Stage 2B (localized) IIC Stage 2C (localized) III Stage 3 NOS(localized) IIIA Stage 3A (localized) IIIB Stage 3B (localized) IIIC Stage 3C (localized) IV Stage 4 (metastasis)
Lung 0 Stage 0 (in situ) IA Stage 1A (localized) IB Stage 1B (localized) IIA Stage 2A (localized) IIB Stage 2B (localized) IIIA Stage 3A (localized) IIIB Stage 3B (localized) IV Stage 4 (metastasis) |
Record patient’s pathologic cancer stage based on the AJCC TNM* staging schema; this may be documented in a staging form that the physician has completed, in a pathology report, etc.; note: cancer is staged pathologically after the patient receives treatment (specifically, surgery)
*American Joint Committee on Cancer – T (tumor) N (node) M (metastasis) |
DISTRESS SCREENING |
||
Did the patient receive distress screening? [Distress screening received] |
0 No 1 Yes |
Record whether the patient received distress screening. Some sources in EHR may include:
|
If the patient did not receive distress screening, what was the reason why? [Why no distress screening received] |
0 Patient declined participation 1 Patient did not have the opportunity to receive screening (e.g., did not return to the hospital, patient expired, other reasons) 2 Other 3 Unknown |
Record why a patient did not receive distress screening |
How many distress screenings did the patient receive? [Number of screenings] |
Enter a number |
Count and record the number of times the patient received distinct distress screenings |
How many days elapsed between the date of the patient’s first cancer encounter and the date of their first distress screening at the facility? [Timing of Distress Screening] |
Enter a number |
Calculate the difference in days between the date of first distress screening and date of the first cancer encounter; it is possible to enter a value of 0, if they occurred on the same day |
What distress tool was used for distress screening? [Distress Tool] |
0 Distress Thermometer 1 Hospital Anxiety and Depression Scale (HADS) 2 Brief Symptom Inventory-18 (BSI-18) 3 Other |
Record the specific distress tool that was used for distress screening |
What score did the patient receive from the distress screening? [Distress Score] |
Enter the number; if there is no score indicated, enter “999” |
Record what score the patient received from the distress screening |
What are some of reasons or problems that the patient identified as being sources of their distress? [Distress Reason] |
0 Practical problems 1 Family problems 2 Emotional problems 3 Spiritual/religious concerns 4 Physical symptoms 5 Substance abuse 6 Other |
Record what problems the patient identified as being sources of their distress, based on the distress thermometer problem list or similar documents/resources; reference the NCCN distress thermometer problem list for how to categorize specific problems |
Was the distress screening that the patient received associated with a “pivotal point” in the patient’s cancer care? [Distress screening point] |
0 Time of diagnosis 1 First visit with a medical oncologist to discuss treatment 2 Routine visit with a radiation oncologist 3 Post-chemotherapy follow-up visit 4 Post-surgical visit 5 Transitions during treatment 6 Transitions off treatment 7 Referral to palliative care 8 Other |
Indicate if the patient was given distress screening as part of a “pivotal point” in their cancer care; review the date distress screening was given and compare it to dates that the patient received cancer care, such as the date of diagnosis and dates of treatment |
Where did the patient receive distress screening? [Distress Screening Location] |
0 Radiation department 1 Chemotherapy infusion center 2 In-patient Medical Oncology 3 In-patient Surgical Oncology 4 Out-patient Medical Oncology 5 Out-patient Surgical Oncology 6 Other |
Indicate where in the hospital the patient received distress screening |
ASSESSMENT* |
||
*It is possible to record information about multiple assessments that the patient receives, based on their first distress screening |
||
Did the patient actually receive an assessment, following distress screening? [Assessment received] |
0 No, reason unknown 1 No, patient refused 2 No, patient did not need/was not referred for assessment 3 Yes |
Indicate whether the patient actually received an assessment following distress screening |
How many days elapsed between the date of the patient’s first cancer encounter and the date of the assessment that they received based on the results of distress screening at the facility? [Timing of assessment [1-5]] |
Enter a number |
Calculate the difference in days between the date of the assessment that the patient received based on the results of distress screening and date of the first cancer encounter; it is possible to enter a value of 0, if they occurred on the same day |
What is the role of the staff person who administered the assessment following distress screening? [Assessment staff] |
1 Oncology Social Worker 2 Nurse or Nurse Navigator 3 Physician 4 Behavioral Health (e.g., mental health professional, including Psychiatrist) 5 Spiritual Care Provider/Chaplain 6 Patient Navigator (e.g., lay or volunteer only) 7 Case Manager/Care Coordinator 8 Nutrition/Dietary (e.g., RD, LD) 9 Outpatient Rehab (e.g., PT,OT,SLP,AuD) 10 Other |
Indicate what staff person administered the assessment to the patient following distress screening |
What mode of contact was used for the assessment between the assessor (social worker or otherwise) and the patient? [Assessment mode] |
1 Face to Face 2 Telephone 3 Email 4 Text 5 Patient Portal 6 Letter 7 Other |
Indicate how the patient received the assessment following distress screening |
INTERVENTION/SERVICES* |
||
*It is possible to record information about multiple interventions/services that the patient is referred to and receives, based on their first distress screening |
||
Number of Interventions/Services |
|
|
Did the patient receive a referral for intervention/services following distress screening and assessment? [Referral for intervention/services] |
1 No – no needs were identified 2 No – patient declined further services 3 No – patient referred for psychosocial assessment only 4 Yes |
Indicate whether the patient received a referral for intervention/services following assessment |
How many days elapsed between the date of the patient’s first cancer encounter and the date they received a referral based on the results of distress screening at the facility? [Timing of referral for intervention/services] |
Enter a number |
Calculate the difference in days between the date the patient received a referral for intervention/services based on the results of distress screening and date of the first cancer encounter; it is possible to enter a value of 0, if they occurred on the same day |
If the patient received a referral for intervention/services, who were they referred to for intervention/services? [Referral for intervention/services staff] |
1 Oncology Social Worker 2 Nurse or Nurse Navigator 3 Physician 4 Behavioral Health (e.g., mental health professional, including Psychiatrist) 5 Spiritual Care Provider/Chaplain 6 Patient Navigator (e.g., lay or volunteer only) 7 Case Manager/Care Coordinator 8 Nutrition/Dietary (e.g., RD, LD) 9 Outpatient Rehab (e.g., PT,OT,SLP,AuD) 10 Other |
Indicate what staff person the patient was referred to for intervention/services |
Did the patient actually receive the intervention/services that they were referred for? [Intervention/services given] |
0 No 1 Yes |
Indicate whether the patient actually received the intervention/services that they received a referral for |
How many days elapsed between the date of the patient’s first cancer encounter and the date the patient received an intervention/service based on the results of distress screening at the facility? [Timing of intervention/services] |
Enter a number |
Calculate the difference in days between the date the patient received an intervention/service based on the results of distress screening and date of the first cancer encounter; it is possible to enter a value of 0, if they occurred on the same day |
If the patient actually received an intervention/services, what type of intervention/services did they receive? [Intervention/service type] |
|
Indicate what types of intervention/services the patient received as a result of the distress screening and assessment, as documented in EHR |
If the patient actually received an intervention/services, did they receive ongoing/repeat visits for intervention/services? [Repeat visits for intervention/services] |
0 No 1 Yes |
Indicate whether the patient received ongoing/repeat visits for intervention services; ongoing/repeat visits are defined as any visits that occur following the first visit for the intervention/services the patient was referred to |
OTHER |
||
Does the patient have any diagnoses or history related to mental health-related conditions? [Mental health status] |
0 No 1 Yes |
Indicate whether patient has any diagnoses or a history of conditions such as depression, suicidal ideation, anxiety, and post-traumatic stress |
What is the patient’s current smoking status? [Smoking status] |
0 Non-smoker 1 Ever smoker 2 Current smoker 3 Recent quitter 4 Former smoker |
Record patient’s smoking status, as indicated in a designated smoking status field or in their physical exam or history notes |
Did the provider ask the patient about their smoking status? [Smoking status from provider] |
0 No 1 Yes 2 Unknown/Not applicable |
Indicate whether the provider asked the patient specifically about their smoking status during their cancer care |
If the patient is a smoker, did the provider refer the patient to a cessation program or similar intervention? [Referral for smoking cessation] |
0 No 1 Yes 2 Not applicable – patient is not a current smoker 3 Unknown |
Indicate whether the provider referred the patient to a cessation program or similar program, or provided any information about quitting smoking to the patient |
Did the provider ask the patient if they recently attempted to quit smoking? [Quit attempt from provider] |
0 No 1 Yes 2 Patient never smoked 3 Unknown |
Indicate whether the provider asked the patient if they made a recent attempt to quit smoking |
How many times did the patient visit the emergency department (ED) within a six-month window after they received distress screening (or should have received distress screening according to the protocol)? [ED VISIT] |
Enter a number |
Review the information provided about the patient’s ED visits and count the number of ED visits the patient had within 6 months after they received their first distress screening or should have received distress screening according to protocol; for example, if the protocol indicates patients should receive distress screening at diagnosis, use that date as the start date; count all ED visits, including those outside the institution |
How many times was the patient admitted for hospitalization within a six-month window after they received distress screening (or should have received distress screening according to the protocol)? [INPATIENT ADMISSIONS AND/OR DISCHARGES] |
Enter a number |
Review the information provided about the patient’s admissions to the hospital and count the number of admissions the patient had within 6 months after they received their first distress screening or should have received distress screening according to protocol; for example, if the protocol indicates patients should receive distress screening at diagnosis, use that date as the start date; count all inpatient admissions, including those outside the institution |
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| Author | Rohan, Elizabeth A. (CDC/ONDIEH/NCCDPHP) |
| File Modified | 0000-00-00 |
| File Created | 2021-01-15 |
© 2026 OMB.report | Privacy Policy