Summary of Benefits and Coverage
Summary of Benefits and Coverage and Uniform Glossary Required Under the Affordable Care Act
Coverage_examples_calculator instructions April 2017
Summary of Benefits and Coverage
OMB: 1210-0147
Coverage Examples Cost Sharing Calculator
Information Packet
March 29, 2016
Revision: 02.07.02
Document Number: RTI.CCIIO.CECSC.02.07.02
Contact Number:
Prepared for:
Centers for Medicare & Medicaid
Services (CMS)
Center for Consumer Information & Insurance
Oversight
Prepared by:
RTI International
Revision History
Revision |
Date |
Revisions |
02.04.XX.02 |
2/9/2016 |
Changed references to “beneficiary” to “subscriber” |
02.05.XX.01 |
2/19/2016 |
Changed revision number to conform to version 02.05 of the
calculator |
2.07.02 |
3/29/2016 |
Added material to § |
Table of Contents
1.0 Purpose and Construction 1
2.0 Using the Coverage Examples Cost Sharing Calculator 1
3.2 The MANUAL_INPUT Worksheet 3
3.3 The MULTIPLE_PLAN_MODE worksheet 5
3.4 The RESULTS_SUMMARY worksheet 6
3.5 The MATERNITY_SUMMARY, DIABETES_SUMMARY and FRACTURE_SUMMARY worksheets 8
3.7 The LINE_ITEM worksheets 14
4.0 Plan Benefit Parameters and the BENEFIT_DESIGN worksheet 15
5.1 Browsing and reviewing Multi-Plan Mode input data 21
5.2 Generating output in Multi-Plan Mode 21
Appendix A: Overview of the Coverage Examples Calculator Logic 22
Phase 1: Obtain the allowed amount 22
Phase 2: Determine whether the claim is for a covered service 22
Phase 3: Apply the monthly and annual coverage limits 22
Phase 4: Apply the required Co-payment or Co-insurance 23
Phase 5: Apply the required deductible 23
Phase 6: Apply the out-of-pocket limit 23
Phase 7: Calculate the subscriber and the plan payment 24
Phase 8: Allocate the subscriber payment to summary aggregation categories 24
Appendix B: PLAN_INPUT_DATA external data file specifications 26
Appendix C: PLAN_OUTPUT_DATA external data file 32
1.0 Purpose and Construction
The Coverage Examples Cost Sharing Calculator (CECSC) is a tool that can be used by health plans to estimate the out-of-pocket expenditure under a benefit package for treatment of three stylized examples: management of stable type 2 diabetes; an uncomplicated pregnancy with a vaginal birth; and a simple foot fracture.
This coverage example calculator makes several assumptions which may not be valid for all plan designs.
The coverage example calculator makes the following assumptions:
The benefit package covers maternity care, diabetes care, and simple fracture care. If the plan does not cover these conditions, the coverage example calculator cannot be used for the non-covered condition;
Consumer out-of-pocket costs do not include premiums.
The condition was not excluded as a pre-existing condition.
The only medical expense incurred by the subscriber was for treatment of the specified condition. There are no medical expenses for any member covered under the plan or policy other than those listed.
The calculator treats each condition independently of the others. (For example, the calculator does not calculate the subscriber’s out-of-pocket cost if she is both diabetic and experiences an uncomplicated fracture.)
All care is in-network and considered first tier (or the tier associated with the lowest level of cost sharing), for those products that incorporate tiered provider networks.
All services occur in same policy period.
All prior authorizations are obtained.
All services are deemed medically necessary.
All costs (allowed amount, sample care costs, member costs) greater than $100 are rounded to the nearest hundred dollars.
All costs (allowed amount, sample care costs, member costs) less than $100 are rounded to the nearest ten dollars.
All medications are covered as generic equivalents if available.
If the plan has a wellness program that varies the deductibles, copayments, coinsurance, or coverage for any of the services listed in a treatment scenario, the benefit design that is applied reflect the cost-sharing required assuming that the patient does NOT participate in the wellness program.
If your plan design differs significantly from these assumptions, the estimated consumer out-of-pocket cost may be inaccurate. In such a case, the user can alter the coverage calculator to make it more accurate. For example, if your plan covers diabetes supplies under the prescription drug benefit, a user can modify the calculator to apply prescription drug cost sharing to those items. Alternatively, the plan can use a coverage calculator that it develops using as inputs the schedules of services provided and the schedule of allowed amounts that are included in the cost sharing calculator.
The CECSC is a macro-enabled Excel™ workbook. The user must enable macros.
2.0 Using the Coverage Examples Cost Sharing Calculator
The CECSC can be used in two different modes. When the workbook is first opened, the WELCOME worksheet is displayed and Mode is selected.
In the Single Plan Mode a user enters the characteristics of a single plan, and then runs the results of the calculator. In Single Plan Mode a user can also add plans one at a time and then export an output file for all of the plans that the user has entered.
In the Multi-Plan Mode a user imports (or copies) data from an external file for a set of plans and then runs the calculator to produce an output file. In Multi-Plan Mode a user can also browse and review the results for each plan before creating the output file.
3.0 Technical Overview
The CECSC has 4 core worksheets that the user interacts with:
The WELCOME worksheet in which the user chooses either the Single Plan or Multi-Plan mode.
The MULTIPLE_PLAN_MODE worksheet in which the user chooses the method that will be used to enter data for multiple plans.
The BENEFIT_DESIGN worksheet in which the user enters the benefit design parameters (i.e., type of cost sharing, deductible amounts, coinsurance rates, copayment amounts, coverage limits, etc.)
The RESULTS_SUMMARY worksheet which displays the estimated cost-sharing under the specified benefit design for each of the standardized coverage examples.
From the RESULTS_SUMMARY worksheet, the user can navigate to a set of three worksheets for each of the coverage examples. Specifically, from the Maternity Example section of the RESULTS_SUMMARY worksheet the user can navigate to:
The MATERNITY_SUMMARY worksheet which shows the allowed amount, the amount of the plan payment, and the amount of the subscriber payment for the maternity coverage example.
The MATERNITY_TIMELINE worksheet which shows the claim-by-claim development of the consumer cost sharing amount.
The MATERNITY_LINE_ITEM worksheet which shows the allowed amount for each of the items and services that are included in the coverage example.
From the Diabetes Type 2 section of the RESULTS_SUMMARY worksheet the user can navigate to:
The DIABETES_SUMMARY worksheet which shows the allowed amount, the amount of the plan payment, and the amount of the subscriber payment for the Type 2 Diabetes coverage example.
The DIABETES_TIMELINE worksheet which shows the claim-by-claim development of the consumer cost sharing amount.
The DIABETES_LINE_ITEM worksheet which shows the allowed amount for each of the items and services that are included in the coverage example.
From the Foot Fracture Example section of the RESULTS_SUMMARY worksheet the user can navigate to:
The FRACTURE_SUMMARY worksheet shows the allowed amount, the amount of the plan payment, and the amount of the subscriber payment for the foot fracture coverage example.
The FRACTURE_TIMELINE worksheet which shows the claim-by-claim development of the consumer cost sharing amount.
The FRACTURE_LINE_ITEM worksheet which shows the allowed amount for each of the items and services that are included in the coverage example.
In addition to these worksheets, the CECSC has two worksheets that are used to store the input and output data when the tool is being used in multi-plan mode.
The PLAN_INPUT_DATA worksheet which holds the benefit design parameters for each of the plans that have been entered.
The PLAN_OUTPUT_DATA worksheet which holds the output data for each of the plans that have been entered.
Each of these worksheets is described in the following sections.
3.1 The WELCOME worksheet
On the WELCOME worksheet, which displays when the tool is opened, the user will select either the Single Plan Mode or the Multi-Plan Mode.
To select the Single Plan Mode, click the Single Plan Mode button. The BENEFIT_DESIGN worksheet will then be displayed, allowing the user to enter the parameters for a single plan or multiple plans one at a time.
To select the Multi-Plan Mode, click the Multi-Plan Mode button. The MULTIPLE_PLAN_MODE worksheet will then be displayed, allowing the user to select the method that will be used to load data for multiple plans.
3.2 The MANUAL_INPUT Worksheet
The BENEFIT_DESIGN worksheet is used to enter the benefit design parameters for a plan.
At the top of the worksheet are several navigation buttons that allow a user to navigate between plans (if more than one plan has been created and saved), to clear or reset the benefit parameters for the displayed plan, to update the benefit parameters for the displayed plan, or to save the displayed plan as a new plan.
The Prev Plan and Next Plan buttons allow a user to navigate between plans (if more than one plan has been created and saved). If any changes were made to the parameters of the plan after it was loaded into the BENEFIT_DESIGN worksheet, a dialog box will prompt the user to save the changed parameters:
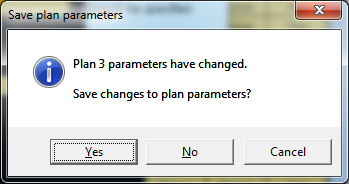
Clicking the Yes button will save the updated parameters for the plan. Clicking the No button will discard the changes to the parameters to the current plan and load the parameters for the next plan into the BENEFIT_DESIGN worksheet. Clicking the Cancel button will allow the user to continue reviewing or editing the updated parameters for the current plan before deciding to load a different plan.
Clicking the Clear button will reset the parameters for the plan that is currently loaded into the BENEFIT_DESIGN worksheet to the default parameters.
Clicking the Update button will save the parameters for the plan that is currently loaded into the BENEFIT_DESIGN worksheet.
Clicking the Save As button will save the parameters for the plan that is currently loaded into the BENEFIT_DESIGN worksheet as a new plan, increment the number of plans that are available, and load the parameters for the newly created plan.
Clicking the Run Calculator button will display the RESULTS_SUMMARY worksheet.
The Multi-Plan Mode button in the upper right corner of the worksheet allows a user to switch to Multi-Plan Mode.
Section 4.0 discusses the entry of plan parameter data into the BENEFIT_DESIGN worksheet.
3.3 The MULTIPLE_PLAN_MODE worksheet
Multi-Plan Mode allows a user to load data for multiple plans into the calculator, run the calculator for all loaded plans, and generate an output file that contains the calculated cost sharing for each of the scenarios for each of the plans.
The MULTIPLE_PLAN_MODE worksheet allows the user to select the method that will be used to load data for multiple plans. The three options are:
To import data from an external file to be used in the calculator. This data must be of a form readable to the program. Text files (.txt) should be delimited by tabs in order to be read into the program.
To copy and paste data from an external data file (such as an Excel worksheet) into the PLAN_INPUT_DATA worksheet.
To enter data for each plan, one at a time, in Single Plan Mode and save the data to the input data worksheet.
The Single Plan Mode button in the lower left corner of the worksheet allows a user to switch to Single Plan Mode. (This will also occur if the user clicks the Option 3 button.)
3.4 The RESULTS_SUMMARY worksheet
The RESULTS_SUMMARY worksheet displays for a plan the estimated cost sharing that is calculated by the CECSC.
Several navigation buttons are provided at the top of the worksheet. The View Input Data button will display the PLAN_INPUT_DATA worksheet, which lists the benefit parameters for each of the plans that has been loaded into to CECSC. The View Output Data button will display the PLAN_OUTPUT_DATA worksheet.
The Plan Parameters button will navigate to the BENEFIT_DESIGN worksheet which will display the benefit design parameters for the plan shown on the RESULTS_SUMMARY worksheet.
The Prev Plan and Next Plan buttons allow a user to navigate between plans (if more than one plan has been created and saved).
The Export Data button will run the calculator and export the output data for all loaded plans to an external file.
Within the section of the RESULTS_SUMMARY worksheet for each of the coverage examples, there are three buttons.
The Detail button will display more detailed data on the calculated cost sharing amounts. For example, in the Maternity Example:
Clicking the Detail button will display the MATERNITY_SUMMARY worksheet.
Clicking the Time Line button will display the MATERNITY_TIMELINE worksheet which shows the claim-by-claim development of the consumer cost sharing amount.
Clicking the Line Item button will display the MATERNITY_LINE_ITEM worksheet which shows the allowed amount for each of the items and services that are included in the coverage example.
Each of the buttons in the other examples works in a similar way.
If the RESULTS_SUMMARY worksheet displays “ERROR” in the calculated cost sharing amounts, it means that there is an uncorrected error in the BENEFIT_DESIGN. To identify the error click the Plan Parameters button, which will navigate to the BENEFIT_DESIGN worksheet. The benefit category or other parameter containing the error will be identified on that worksheet.
3.5 The MATERNITY_SUMMARY, DIABETES_SUMMARY and FRACTURE_SUMMARY worksheets
The summary worksheets for each of the coverage examples (MATERNITY_SUMMARY worksheet, DIABETES_SUMMARY worksheet and FRACTURE_SUMMARY worksheet) display a summary of the calculated payment amounts including the allowed amounts. These data are informational.
The payment data are organized by the benefit category to which claims are assigned. (See section 4 for additional information on benefit categories.)
3.6 The TIMELINE worksheets
The MATERNITY_TIMELINE worksheet, DIABETES_TIMELINE worksheet and FRACTURE_TIMELINE worksheet are where the cost sharing amounts are calculated. The cost sharing amount is calculated in an 8-stage process that is described in Appendix A. Row 1 of this worksheet identifies the stage (described as a “phase”) that is implemented by the column.
Columns A through G display the scenario’s data on the items and services that were provided to the hypothetical subscriber. The remaining columns correspond to the 8 phases of the process that calculate the consumer cost sharing.
Table 3.6. Descriptive information for the line-item claim
Column |
Column Heading |
Description |
A |
Claim number |
The claim number in chronological sequence of processing. |
B |
Date |
The date the item or service was rendered. |
C |
Calendar Month |
The calendar month in which the item or service was rendered (Used to apply monthly limits). |
D |
Item or Service Code |
The code for the item or service. Corresponds to the codes for the item or service in column A of the corresponding LINE_ITEM worksheet. |
E |
Description |
The description for the item or service from column F of the corresponding LINE_ITEM worksheet. |
F |
Benefit Category |
The benefit category to which the item or service is assigned. This is given in column E of the corresponding LINE_ITEM worksheet where it can also be changed by the user by making use of the drop-down menu in the relevant cell. |
G |
Cost-sharing type |
The cost sharing type that is assigned to the item or service based on its benefit category (column F) and the benefit parameters for that benefit category that are given in the BENEFIT_DESIGN worksheet. |
Table 3.6.1. Phase 1. Obtain the allowed amount for the item or service
Column |
Column Heading |
Description |
H |
Allowed amount |
The allowed amount for the item or service as given in column G of the corresponding LINE_ITEM worksheet. The allowed amounts cannot be modified by the user. |
Table 3.6.2. Phase 2. Determine whether the claim is for a covered service
Column |
Column Heading |
Description |
I |
Not covered |
The amount of the consumer’s liability (the allowed amount) if the item or service is not covered. |
J |
Covered amount |
The allowed amount, before application of coverage limitations, cost sharing requirements, or out-of-pocket limits if the item or service is covered. This is the starting point for the calculation of the plan liability and the consumer’s out-of-pocket cost for a covered service. |
Table 3.6.3. Phase 3. Apply the monthly and annual coverage limits
Column |
Column Heading |
Description |
K |
Monthly limit |
The limit on the number of claims for the specified item or service that the plan will cover if received in a single calendar month. “None” if the plan does not have monthly coverage limits that apply to the item or service.¹ The monthly limit is determined by the benefit category to which the item or service is assigned (column F) and the parameters for that benefit category specified in the BENEFIT_DESIGN worksheet. |
L |
Prior use (month) |
The number of claims for the specified item or service that have already been submitted and covered by the plan for the month in which the line-item was received. |
M |
subscriber pays because monthly limit exceeded |
The amount that the consumer is required to pay because the monthly limit has already been reached. If the monthly limit has been reached the consumer is responsible for the allowed amount. |
N |
Annual limit |
The limit on the number of claims for the specified item or service that the plan will cover if received in a calendar year. “None” if the plan does not have annual coverage limits that apply to the item or service. The annual limit is determined by the benefit category to which the item or service is assigned (column F) and the parameters for that benefit category specified in the BENEFIT_DESIGN worksheet. |
O |
Prior use (annual) |
The number of claims for the specified item or service that have already been submitted and covered by the plan for the year which the line-item was received.¹ |
P |
subscriber pays because annual limit exceeded |
The amount that the consumer is required to pay because the monthly limit has already been reached. If the annual limit has been reached the consumer is responsible for the allowed amount. |
¹ Note that coverage limits are applied as if the only services that a consumer has received are the services listed in each coverage example.
Table 3.6.4. Phase 4. Apply the required co-payment or co-insurance
Column |
Column Heading |
Description |
Q |
Co-payment amount |
The copayment amount that applies to the item or service based on the benefit category to which the item or service is assigned (column F) and the parameters for that benefit category specified in the BENEFIT_DESIGN worksheet. The copayment amount is shown only if the item or service is covered and the monthly or annual coverage limit has not been reached. |
R |
Co-insurance rate |
The coinsurance rate that applies to the item or service based on the benefit category to which the item or service is assigned (column F) and the parameters for that benefit category specified in the BENEFIT_DESIGN worksheet. |
S |
Co-insurance amount |
The coinsurance amount that applies to the item or service which is equal to the product of the covered amount (column J) and the co-insurance rate (column R) for the item or service. The copayment amount is shown only if the item or service is covered and the monthly or annual coverage limit has not been reached. |
Table 3.6.5. Phase 5. Apply the required deductible
Column |
Column Heading |
Description |
T |
Allowed amount after co-payment or co-insurance |
The difference between the allowed amount for the item or service if no coverage limit had been applied and after the amount of any required copayment or cost sharing has been deducted. The allowed amount after co-payment or co-insurance is zero if the required copayment exceeds the allowed amount. |
U |
Plan deductible applies |
Indicator of whether the plan-level deductible applies to the item or service based on its benefit category (column F) and the cost sharing parameters for that benefit category from the BENEFIT_DESIGN worksheet. |
V |
remaining plan deductible |
The amount of the plan deductible that remains after all previous charges against the plan deductible have been taken. |
W |
subscriber pays toward plan deductible¹ |
The difference between the remaining plan-deductible (column V) and the allowed amount after co-payment or co-insurance (column T). |
X |
Rx deductible applies |
Indicator of whether the Rx deductible applies to the item or service based on its benefit category (column F) and the cost sharing parameters for that benefit category from the BENEFIT_DESIGN worksheet. |
Y |
remaining Rx deductible |
The amount of the Rx deductible that remains after all previous charges against the plan deductible have been taken. |
Z |
subscriber pays toward Rx deductible¹ |
The difference between the remaining Rx deductible (column Y) and the allowed amount after co-payment or co-insurance (column T). |
AA |
deductible C applies |
Indicator of whether Deductible C applies to the item or service based on its benefit category (column F) and the cost sharing parameters for that benefit category from the BENEFIT_DESIGN worksheet. |
AB |
remaining deductible C |
The amount of Deductible C that remains after all previous charges against the plan deductible have been taken. |
AC |
subscriber pays toward deductible C¹ |
The difference between the remaining Deductible C (column AB) and the allowed amount after co-payment or co-insurance (column T). |
AD |
deductible D applies |
Indicator of whether Deductible D applies to the item or service based on its benefit category (column F) and the cost sharing parameters for that benefit category from the BENEFIT_DESIGN worksheet. |
AE |
remaining deductible D |
The amount of Deductible D that remains after all previous charges against the plan deductible have been taken. |
AF |
subscriber pays toward deductible D¹ |
The difference between the remaining Deductible D (column AE) and the allowed amount after co-payment or co-insurance (column T). |
AG |
benefit deductible applies |
Indicator of whether a benefit-category deductible applies to the item or service based on its benefit category (column F) and the cost sharing parameters for that benefit category from the BENEFIT_DESIGN worksheet. |
AH |
remaining benefit deductible |
The amount of any benefit-category deductible that remains after all previous charges against the plan deductible have been taken. |
AI |
subscriber pays toward benefit deductible¹ |
The difference between the remaining benefit-category deductible (column AI) and the allowed amount after co-payment or co-insurance (column T). |
AJ |
subscriber pays toward any deductible¹ |
The amount of the consumer liability under any deductible. Equal to the sum of the amount paid toward the plan deductible, the Rx deductible, deductible C, deductible D, or specific benefit-category deductibles. |
AK |
Covered amount remaining after deductibles |
The difference between the covered amount (column I) for services not subject to annual or monthly coverage limits and the amount of the subscriber’s deductible |
¹ Note that any given item or service is subject to one and only one deductible.
Table 3.6.6. Phase 6. Apply the out-of-pocket limit
Column |
Column Heading |
Description |
AL |
subscriber payment before OPL |
The total year-to-date payments of the subscriber up to and including any payments related to the current claim. |
AM |
OPL applies |
An indicator of whether the out-of-pocket limit applies to this benefit category based on the benefit category to which the item or service is assigned (column F) and the benefit parameters specified for that benefit category in the BENEFIT_DESIGN worksheet |
AN |
amount subject to OPL |
The amount of the subscriber payment before OPL (column AL) if the out-of-pocket limit applies to the item or service (column AM) |
AO |
remaining OPL after subscriber payment |
The difference between the out-of-pocket limit and the amount paid out-of-pocket by the subscriber for items and services that are subject to the out-of-pocket limit |
Table 3.6.7. Phase 7. Calculate the subscriber and the plan payment
Column |
Column Heading |
Description |
AP |
subscriber payment after OOP limit |
If the out-of-pocket limit applies to the item or service the lesser of the amount subject to OPL (column AN) and the subscriber payment before application of the OPL (column AL) |
AQ |
plan payment |
The difference between the covered amount (column F) and the subscriber payment after application of the out-of-pocket limit (column AP) |
Table 3.6.8. Phase 8. Allocate the subscriber payment to the summary aggregation categories
Column |
Column Heading |
Description |
AR |
Not covered |
The amount of the allowed charge if the item or service is not covered |
AS |
Exclusions |
The amount of the allowed charge if the item or service was subject to coverage limitations |
AT |
Subscriber-paid copayment |
The lesser of the co-payment amount (column Q) and the subscriber payment after application of the out-of-pocket limit (column AP) |
AU |
Subscriber-paid coinsurance |
The lesser of the co-insurance amount (column S) and the subscriber payment after application of the out-of-pocket limit (column AP) |
AV |
Subscriber-paid deductible |
The greater of the payment toward deductibles (column AJ) and the difference between the subscriber payment after application of the out-of-pocket limit (column AP) and the subscriber’s co-payment (column Q) and co-insurance amounts (column S) |
3.7 The LINE_ITEM worksheets
The MATERNITY_LINE_ITEM worksheet, DIABETES_LINE_ITEM worksheet and FRACTURE_TIMELINE worksheet contain the list of items and services that appear in the TIMELINE worksheets for each coverage example. The LINE_ITEM worksheets describe each item and service, identify the benefit category (which can be modified by the user by making use of the drop-down menus in column E), and the allowed amount. Table 3.7 describes the columns in these worksheets.
Table 3.7. LINE_ITEM worksheet columns
Column |
Column Heading |
Description |
A |
Item or Service Code |
The code for the item or service. Corresponds to the codes for the item or service in column D of the corresponding TIMELINE worksheet |
B |
Diagnosis Code
|
When applicable an ICD-9 diagnosis code related to the item or service. This is informational. |
C |
CPT©,
HCPCS, or |
The “standard” procedure code for the item or service. This is informational. |
D |
Provider |
The type of provider that typically provides the service. This is informational. |
E |
Benefit Category |
The benefit category to which the item or service is assigned by default. The user can change the benefit category for individual items or services using the drop down menu that is provided in the cells in column E. Note that the user must select one of the 20 benefit categories used in the CECSC. |
F |
Description |
A brief description of the item or service. |
G |
Allowed |
The allowed amount for the item or service. |
H |
Notes |
Brief comments provided for information only. |
I |
Valid Benefit Category |
An indicator that shows whether the benefit category assigned to the item or service in column E is one of the 20 allowed benefit categories. Provided as a check if the user changes the default benefit category assigned to an item or service. |
J |
Timeline Count |
A count of the number of times the item or service (identified by Item or service code (column A) appears in the related TIMELINE worksheet. |
4.0 Plan Benefit Parameters and the BENEFIT_DESIGN worksheet
In the BENEFIT_DESIGN worksheet, the coverage parameters for each coverage category are specified. The coverage parameters include:
The type of cost sharing (cost sharing option) that applies to each benefit category. The CECSC defines 19 standard cost sharing options (see §4.2).
The benefit-level deductible when a coverage option requiring a benefit-deductible is selected.
The co-payment amount when a coverage option requiring a co-payment is selected.
The co-payment amount when a coverage option requiring a co-payment is selected.
The monthly and annual coverage limit that applies to the benefit category.
Whether the benefit category falls under the plan’s out-of-pocket limit.
The plan-level deductibles that apply to the plan. Up to four plan-level deductibles may be specified.
To select a cost sharing option for a benefit category, a user should make use of the drop-down menus that are available when the cell specifying the type of cost sharing that applies is selected for that benefit category. In Single Plan Mode only the allowed cost sharing options can be selected. (See figure 4.1.)
Figure 4.1. Use of drop-down menu to select
cost sharing option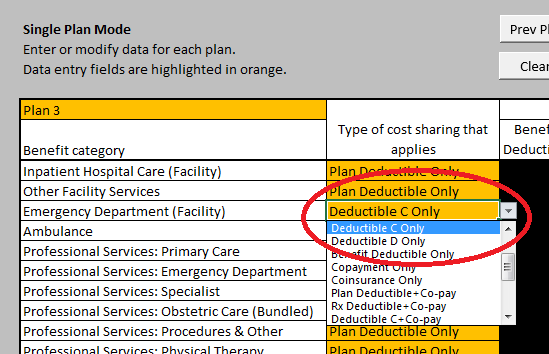
Trying to enter a cost sharing option that is not one of the 19 allowed options will trigger an error dialog shown in Figure 4.2.
Figure 4.2. Error dialog for selection of
invalid cost sharing option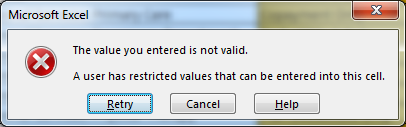
Clicking the Retry button will let the user modify the data that have been entered. Clicking cancel will restore the value that existed before the user tried to enter new data.
Depending on the cost sharing option that is selected, certain parameters either must or must not be specified. Initially these parameters will not have been specified and the BENEFIT_DESIGN worksheet will identify the “warnings” that result. These warnings may include parameters that must be but have not been specified or parameters have been but must not be specified. For example, figure 4.3 shows the warnings that would appear if the cost sharing option for Inpatient hospital care had been changed from Plan Deductible Only to Deductible C plus Co-payment.
Figure 4.3. Warnings associated with
“incomplete” entry of benefit parameters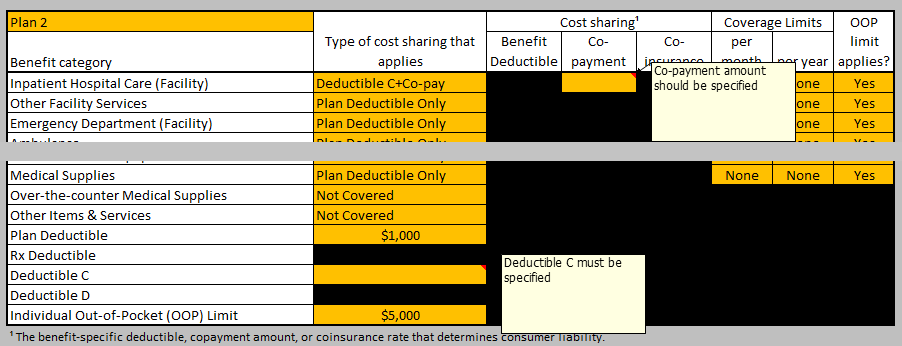
In this example, the user must specify a copayment amount for Inpatient Hospital Care and must specify an amount for Deductible C.
Depending on the cost sharing option that is selected, the other parameters that are required will be dark yellow. Parameters that are not permitted will be black and any data that has been entered will be in red type. When the required data are entered or the prohibited data are deleted the warnings will disappear.
4.1 Benefit Categories
The CECSC assigns claims to one of 20 benefit categories:
Inpatient Hospital Care (Facility)
Other Facility Services
Emergency Department (Facility)
Ambulance
Professional Services: Primary Care
Professional Services: Emergency Department
Professional Services: Specialist
Professional Services: Obstetric Care (Bundled)
Professional Services: Procedures & Other
Professional Services: Physical Therapy
Diagnostic Services: Radiology
Diagnostic Services: Laboratory
Prescription Drugs: Generic
Prescription Drugs: Branded
Over-the-counter Drugs
Preventive Services & Vaccines
Durable Medical Equipment
Medical Supplies
Over-the-counter Medical Supplies
Other Items & Services
Each line item or service code on the LINE_ITEM worksheets is assigned to one of these benefit categories (in column E). The benefit category determines whether a plan covers the item or service, the cost sharing requirements for the item or service under the plan, and what limits the plan applies to coverage for that item or service. A user can customize the benefit categories to which each item or service is assigned and can redefine the benefit categories that are used by the calculator as described in section 4.5.
4.2 Cost Sharing Options
The CECSC uses 19 standard coverage options as described in Table 4.2.
Table 4.2. Standard coverage options
Cost sharing option |
Description |
Not Covered |
The benefit category is not covered by the plan. |
No Cost Sharing |
The benefit category identifies items and services that are covered but that have no required cost sharing. An example would be preventive services. |
Plan Deductible Only |
The benefit category identifies items and services that are covered and that are subject to the plan-level deductible but no coinsurance or copayment. |
Rx Deductible Only |
The benefit category identifies items and services that are covered and that are subject to the prescription drug (Rx) deductible but no coinsurance or copayment. |
Deductible C Only |
The benefit category identifies items and services that are covered and that are subject to a third plan-level deductible that applies to multiple benefit categories but no coinsurance or copayment. |
Deductible D Only |
The benefit category identifies items and services that are covered and that are subject to a fourth plan-level deductible that applies to multiple benefit categories but no coinsurance or copayment. |
Benefit Deductible Only |
The benefit category identifies items and services that are covered and that are subject to a deductible that applies only to the benefit category with no coinsurance or copayment. |
Copayment Only |
The benefit category does not fall under any deductible but does have a copayment. |
Coinsurance Only |
The benefit category does not fall under any deductible but does require a coinsurance payment. |
Plan Deductible+Co-pay |
The benefit category identifies items and services that are covered and that are subject to the plan-level deductible and to a copayment. |
Rx Deductible+Co-pay |
The benefit category identifies items and services that are covered and that are subject to the prescription drug (Rx) deductible and to a copayment. |
Deductible C+Co-pay |
The benefit category identifies items and services that are covered and that are subject to a third plan-level deductible that applies to multiple benefit categories and to a copayment. |
Deductible D+Co-pay |
The benefit category identifies items and services that are covered and that are subject to a fourth plan-level deductible that applies to multiple benefit categories and to a copayment. |
Benefit Deductible+Co-pay |
The benefit category identifies items and services that are covered and that are subject to a deductible that applies only to the benefit category and to a copayment. |
Plan Deductible+Co-ins |
The benefit category identifies items and services that are covered and that are subject to the plan-level deductible and to a coinsurance payment. |
Rx Deductible+Co-ins |
The benefit category identifies items and services that are covered and that are subject to the prescription drug (Rx) deductible and to a coinsurance payment. |
Deductible C+Co-ins |
The benefit category identifies items and services that are covered and that are subject to a third plan-level deductible that applies to multiple benefit categories and to a coinsurance payment. |
Deductible D+Co-ins |
The benefit category identifies items and services that are covered and that are subject to a fourth plan-level deductible that applies to multiple benefit categories and to a coinsurance payment. |
Benefit Deductible+Co-ins |
The benefit category identifies items and services that are covered and that are subject to a deductible that applies only to the benefit category and to a coinsurance payment. |
Deductible amounts (of any type) must be entered as dollars and cents. Copayment amounts must be entered as dollars and cents. Coinsurance amounts must be entered as values greater than zero and less than 1.00, i.e. 30% must be entered as 0.30 or 30%.
4.3 Coverage limits
Data for coverage limits must be entered for all services that are covered. (Coverage limits cannot be entered for services that are not covered. Doing so will create a warning.)
If no coverage limit applies, “None” must be entered as the monthly and annual coverage limit.
If a monthly but not an annual coverage limit applies, an integer of 1 or greater must be entered in the “per month” coverage limit column and “None” must be entered in the “per year” coverage limit column.
If an annual but not a monthly coverage limit applies, an integer of 1 or greater must be entered in the “per year” coverage limit column and “None” must be entered in the “per month” coverage limit column.
If both monthly and annual coverage limits applies, an integer of 1 or greater must be entered in both the “per month” coverage limit column and the “per year” coverage limit column.
4.4 Out-of-pocket Limits
If a benefit category contributes to the out-of-pocket limit, then “Yes” must be entered in the column headed “OOP Limit applies?” If the benefit category does not contribute to the out-of-pocket limit, then “No” must be entered in that column.
If the benefit category is not covered, the out-of-pocket limit column must be left blank.
4.5 Customizing the Benefit Categories
A user may customize the cost calculator to better reflect the way a specific plan covers the items and services specified on the LINE_ITEM worksheets for the three coverage examples. A user can customize the benefit categories to which each item or service is assigned, and can redefine the benefit categories the calculator uses.
4.5.1 Reassigning the Benefit Category for an item or service
The calculator allows each item or service listed in the LINE_ITEM worksheets for the three coverage examples to be assigned to one of 20 benefit categories. A user can change the benefit category to which an item or service is assigned on the LINE_ITEM worksheet.
For example, by default the coverage calculate assigns diabetic test strips to the Medical Supplies benefit category. However, a user may change that category so that test trips are covered under the Over-the-counter Medical Supplies benefit category or under the Other Items & Services benefit category using the drop-down list of benefit categories:
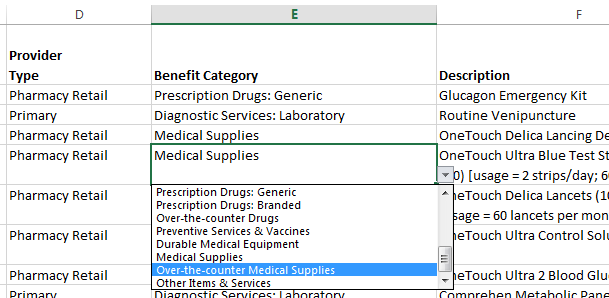
Note, a user must select one of the 20 listed benefit categories. These are the benefit categories that are listed on the BENEFIT_DESIGN worksheet.
Note that the reassignment of an item or service to a benefit category using the LINE_ITEM worksheet will apply only to the item or service in the coverage example. For example, influenza vaccination is a line item in both the diabetes and maternity coverage examples. Changing the benefit category to which influenza vaccination is assigned in the DIABETES_TIME_LINE will not change the benefit category to which influenza vaccination is assigned in the MATERNITY_TIME_LINE.
4.5.2 Redefining the Benefit Categories
Any of the 20 benefit categories can be redefined in the calculator. The only limitation imposed by the calculator is that the number of benefit categories cannot exceed 20. However, if a plan needs to define a specific benefit category for Diabetic Supplies it can do so by following a two-step procedure.
Step one is to change the labels that are used to identify the benefit categories on the BENEFIT_DESIGN worksheet. For example, a user might want to use the Other Items & Services benefit category:
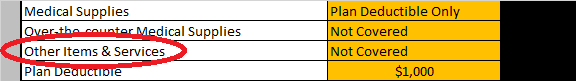
to identify Diabetes Supplies:
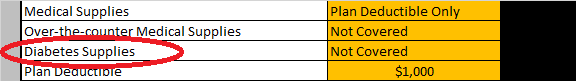
This changes makes the benefit category Diabetes Supplies available for use in the calculator. However, it also means that the benefit category Other Items & Services is no longer available and any item or service that is assigned to the Other Items & Services benefit category in a LINE_ITEM worksheet must be re-assigned either to Diabetes Supplies or to another of the benefit categories listed on the BENEFIT_DESIGN worksheet.
Step 2 is to change the benefit category for the items and services that are to be paid under the new Diabetes Supplies benefit category. In this example, the user will modify the benefit categories to which the items on the DIABETES_LINE_ITEM worksheet are assigned. These items and services may include lancing devices, test strips, lancets, control solutions, and syringes. The user must change the benefit category for each of those items to Diabetes Supplies using the drop-down menu.
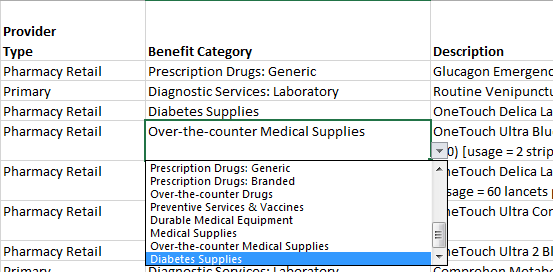
The re-designated benefit category Diabetes Supplies will now be an available option in the drop-down list.
A user can, in fact, redefine all 20 of the benefit categories to better match the categories that the plan uses. However, in this case the user will need to make extensive revisions to the TIME_LINE worksheets so that every item or service is correctly mapped to one of the newly defined benefit categories.
CAUTION: If a user changes the designation for a benefit category that is used by multiple coverage examples (for example, both the FRACTURE example and the DIABETES example), any item or service in any of the LINE_ITEM schedules that was assigned to the benefit category as it was originally designated will need to be reassigned either to the new category or to another available category.
5.0 Multi-Plan Mode
When used in Multi-Plan Mode, the CECSC allows a user to populate the PLAN_INPUT_DATA worksheet with benefit parameters for multiple plans.
This worksheet may be populated by importing a tab-separated text file containing the benefit parameter data (see Appendix B) or by directly entering data on the PLAN_INPUT_DATA worksheet. (Directly entering data into the PLAN_INPUT_DATA worksheet is not recommended as 146 variables or columns must be completed for each plan.)
Figure 5.0. PLAN_INPUT_DATA worksheet
The first 7 rows of the PLAN_INPUT_DATA worksheet contain a button that will run the calculator and generate output for the plans whose parameters are listed starting on row 8. Rows 6 and 7 are the “header” for the plan parameter data.
WARNING: Do NOT separate groups of plans by using a blank row. A blank row is interpreted by the CECSC as signaling the end of the entered data. Any data below a blank row will be ignored by the CECSC.
The plan parameter data are divided into 21 groups.
Plan-level parameters (Columns A through F): the plan identifier, the plan deductible, the Rx deductible, Deductible C, Deductible D, and the out-of-pocket limit (if any) that applies to the plan.
Inpatient hospital care coverage parameters (columns G through M):
The cost sharing option or type (column G)
Benefit deductible (if required by the cost sharing option) (column H)
Copayment amount (if required by the cost sharing option) (column I)
Coinsurance rate (if required by the cost sharing option) (column J)
The monthly coverage limit (if required by the cost sharing option) (column K)
The annual coverage limit (if required by the cost sharing option) (column L)
Whether the out-of-pocket limit applies(column M)
Other Facility Services coverage parameters (columns N through T)
Emergency Department (Facility) (columns U through AA)
Ambulance (columns AB through AH)
Professional Services: Primary Care (columns AI through AO)
Professional Services: Emergency Department (columns AP through AV)
Professional Services: Specialist (columns AW through BC)
Professional Services: Obstetric Care (Bundled) (columns BD through BJ)
Professional Services: Procedures & Other (columns BK through BQ)
Professional Services: Physical Therapy (columns BR through BX)
Diagnostic Services: Radiology (columns BY through CE)
Diagnostic Services: Laboratory (columns CF through CL)
Prescription Drugs: Generic (columns CM through CS)
Prescription Drugs: Branded (columns CT through CZ)
Over-the-counter Drugs (columns DA through DG)
Preventive Services & Vaccines (columns GH through DN)
Durable Medical Equipment (columns DO through DU)
Medical Supplies (columns DV through EB)
Over-the-counter Medical Supplies (columns EC through EI)
Other Items & Services (columns EJ through EP)
An external data file that will be imported using Multi-Plan Mode Option 1 must be a tab-separated value file consisting of 146 “fields” or “variables” corresponding to the above.
5.1 Browsing and reviewing Multi-Plan Mode input data
Once the plan parameter data for multiple plans have been loaded into the PLAN_INPUT_DATA worksheet, the BENEFIT_DESIGN worksheet can be used to browse and review the plan input data. As each plan is loaded, error checking will be performed and any errors will be identified by “warning” notices in the BENEFIT_DESIGN worksheet.
If errors exist in the input data for a plan, the output data will simply indicate ERROR.
5.2 Generating output in Multi-Plan Mode
To generate output in Multi-Plan Mode the user will click the Run Calculator button that is found on the PLAN_INPUT_DATA worksheet or the PLAN_OUTPUT_DATA worksheet, or the user can click the View Output Data button or the Export Data button on the RESULTS_SUMMARY worksheet.
Appendix A: Overview of the Coverage Examples Calculator Logic
The Coverage Examples Cost Sharing Calculator (the Calculator) calculates the subscriber and plan payment for a claim (i.e., the claim for a service provided on a specified date) for a subscriber with self-only coverage in eight phases:
Phase 1: Obtain the allowed amount.1
Phase 2: Determine whether the claim is for a covered service.
Phase 3: Apply the monthly and annual coverage limits.
Phase 4: Apply the required Co-payment or Co-insurance.
Phase 5: Apply the required deductible.
Phase 6: Apply the out-of-pocket limit.
Phase 7: Calculate the subscriber and the plan payment.
Phase 8: Allocate the subscriber payment to summary aggregation categories.
The following sections describe the Calculator logic for each phase.
Phase 1: Obtain the allowed amount
For each line item in the so-called “timeline”, the Calculator looks up the allowed amount for the Item or Service Code in the associated “line item” charge schedule.
Phase 2: Determine whether the claim is for a covered service
For the line item, the Calculator looks up the benefit category (broadly speaking, the benefit that the line item falls under) that applies to the Item or Service Code in the associated “line item” charge schedule. It then looks up the coverage that applies to the benefit category.
Phase 3: Apply the monthly and annual coverage limits
Based on the coverage that applies to the benefit category, the Calculator looks up the monthly limit that applies to the line item. It calculates the total number of claims for the same service that have been provided during the same month as the current claim. If the total number of claims is less than the monthly limit or if the plan does not apply a monthly limit, the claim is covered by the plan and nothing accrues to the subscriber. If the total number of claims equals or exceeds the monthly limit, the allowable charge accrues to the subscriber.
Based on the coverage that applies to the benefit category, the Calculator looks up the annual limit that applies to the line item. It calculates the total number of claims for the same service that have been provided during the same year as the current claim. If the total number of claims is less than the annual limit or if the plan does not apply an annuallimit, the claim is covered by the plan and nothing accrues to the subscriber. If the total number of claims equals or exceeds the annual limit, the allowable charge accrues to the subscriber.
Phase 4: Apply the required Co-payment or Co-insurance
If the line-item is covered by the plan and is not subject to the monthly or annual limit, the Calculator looks up the co-payment that applies to the line item based on the coverage that applies to the benefit category. If the copayment amount is greater than zero, the amount of the copayment accrues to the subscriber.
If the line item is covered by the plan and is not subject to the monthly or annual limit, the Calculator looks up the co-insurance rate that applies to the line item based on the coverage that applies to the benefit category. If the insurance rate is greater than zero, the amount of the coinsurance that accrues to the subscriber is calculated by multiplying the coinsurance rate by the allowable amount.
Phase 5: Apply the required deductible
The amount of the allowed amount that is subject to the deductible is equal to the allowed amount less any copayment or coinsurance that has accrued to the subscriber.
The application of the appropriate deductible proceeds in five stages corresponding to each of the five deductibles that may apply to a line item. The benefit design may subject each line item to one of five deductibles or to no deductible. These five deductibles are:
The overall plan deductible;
The prescription drug deductible;
An optional deductible (e.g., that applies to Emergency Services) referred to as deductible C;
An optional deductible (e.g., that applies to Physician Services) referred to as deductible D;
A deductible that applies only to the benefit category.
The calculator determines whether the overall plan deductible applies to the line item based on the benefit category for the line item. If the overall plan deductible applies, the calculator obtains the plan deductible and deducts any payments that counted toward the plan deductible for items and services that were received prior to the line-item being adjudicated. If the remaining plan deductible is greater than the allowed amount that is subject to the deductible, the amount subject to the deductible accrues to the subscriber. If the remaining plan deductible is less than the allowed amount that is subject to the deductible, the amount of the remaining plan deductible accrues to the subscriber.
This same procedure is repeated for each of the remaining deductibles.
Phase 6: Apply the out-of-pocket limit
The Calculator computes the amount of the subscriber’s out-of-pocket payment, which is equal to the amount of any liability that accrued to the subscriber for the line item as a result of:
The application of the monthly and annual limits on coverage;
The application of copayment and coinsurance; and,
The application of the plan deductible, prescription drug deductible, optional deductible C, optional deductible D, and benefit deductibles.
This is the amount of the subscriber’s out-of-pocket liability for the line item prior to the application of the out-of-pocket limit.
The Calculator determines, based on the benefit category that applies to the line item, whether the claim is subject to the out-of-pocket limit.
If the line-item is subject to the out-of-pocket limit, the calculator compares the subscriber liability prior to application of the out-of-pocket limit to the remaining allowed out-of-pocket expenditure. The subscriber’s liability for the claim is the lesser of the amount of the remaining allowed out-of-pocket expenditure and the amount of the subscriber’s liability prior to the application of the out-of-pocket limit.
Phase 7: Calculate the subscriber and the plan payment
The Calculator compares the amount of the subscriber’s liability after application of the out-of-pocket limit to the allowed amount (see Phase 1). If the subscriber’s liability is less than the allowed amount, the plan’s liability is equal to the difference between the allowed amount and the subscriber’s liability. If the subscriber’s liability is equal to or greater than the allowed amount, the plan’s liability is zero.
Phase 8: Allocate the subscriber payment to summary aggregation categories
The amount of any subscriber liability is allocated to the reporting categories (i.e., not covered or exclusions, coinsurance, copayment, or deductibles) by comparing the amount of the subscriber’s liability that is determined at each step to the amount of the subscriber’s liability after application of the out-of-pocket limit.
If the subscriber is liable for the claim because the monthly or annual limits have been exceeded, the amount of the allowed amount up to the amount of the total subscriber liability after application of the out-of-pocket limit is allocated to “exclusions”.
If the subscriber was not liable for the claim because the monthly or annual limits have been exceeded, and the amount of copayment is less than or equal to the amount of the total subscriber liability after application of the out-of-pocket limit, the amount of the copayment up to the total subscriber liability after application of the out-of-pocket limit is allocated to “co-payments”.
If the subscriber was not liable for the claim because the monthly or annual limits have been exceeded, and the amount of coinsurance is less than or equal to the amount of the total subscriber liability after application of the out-of-pocket limit, the amount of the coinsurance up to the total subscriber liability after application of the out-of-pocket limit is allocated to “co-insurance”.
If the subscriber was not liable for the claim because the monthly or annual limits have been exceeded, and the amount of the allowed amount that was charged against deductibles is less than or equal to the amount of the total subscriber liability after application of the out-of-pocket limit less the amount of any coinsurance or deductible, the amount of the allowed amount that was charged against deductibles up to the total subscriber liability after application of the out-of-pocket limit is allocated to “deductibles”.
Appendix B: PLAN_INPUT_DATA external data file specifications
Table B-1 specifies the required data elements and formats for an external data file of plan parameters. This file must have no header and no trailer. It should contain only plan parameter data.
Table B-1. Layout of PLAN_INPUT_DATA external data file
Column |
Data category |
Variable |
Allowable values |
1 |
Plan-level parameters |
PLAN_ID |
Alphanumeric |
2 |
Plan-level parameters |
Plan deductible |
Blank or numeric |
3 |
Plan-level parameters |
Rx deductible |
Blank or numeric |
4 |
Plan-level parameters |
Deductible C |
Blank or numeric |
5 |
Plan-level parameters |
Deductible D |
Blank or numeric |
6 |
Plan-level parameters |
OOP Limit |
Blank or numeric |
7 |
Inpatient Hospital Care (Facility) |
Cost sharing Type |
See note 1 |
8 |
Inpatient Hospital Care (Facility) |
Benefit Deductible |
Blank or numeric |
9 |
Inpatient Hospital Care (Facility) |
Co-payment |
Blank or numeric |
10 |
Inpatient Hospital Care (Facility) |
Co-insurance |
Blank or numeric |
11 |
Inpatient Hospital Care (Facility) |
Monthly Limits |
Blank, "None" or numeric |
12 |
Inpatient Hospital Care (Facility) |
Annual Limits |
Blank, "None" or numeric |
13 |
Inpatient Hospital Care (Facility) |
OOP Limit Applies |
Blank, "Yes" or "No" |
14 |
Other Facility Services |
Cost sharing Type |
See note 1 |
15 |
Other Facility Services |
Benefit Deductible |
Blank or numeric |
16 |
Other Facility Services |
Co-payment |
Blank or numeric |
17 |
Other Facility Services |
Co-insurance |
Blank or numeric |
18 |
Other Facility Services |
Monthly Limits |
Blank, "None" or numeric |
19 |
Other Facility Services |
Annual Limits |
Blank, "None" or numeric |
20 |
Other Facility Services |
OOP Limit Applies |
Blank, "Yes" or "No" |
21 |
Emergency Department (Facility) |
Cost sharing Type |
See note 1 |
22 |
Emergency Department (Facility) |
Benefit Deductible |
Blank or numeric |
23 |
Emergency Department (Facility) |
Co-payment |
Blank or numeric |
24 |
Emergency Department (Facility) |
Co-insurance |
Blank or numeric |
25 |
Emergency Department (Facility) |
Monthly Limits |
Blank, "None" or numeric |
26 |
Emergency Department (Facility) |
Annual Limits |
Blank, "None" or numeric |
27 |
Emergency Department (Facility) |
OOP Limit Applies |
Blank, "Yes" or "No" |
28 |
Ambulance |
Cost sharing Type |
See note 1 |
29 |
Ambulance |
Benefit Deductible |
Blank or numeric |
30 |
Ambulance |
Co-payment |
Blank or numeric |
31 |
Ambulance |
Co-insurance |
Blank or numeric |
32 |
Ambulance |
Monthly Limits |
Blank, "None" or numeric |
33 |
Ambulance |
Annual Limits |
Blank, "None" or numeric |
34 |
Ambulance |
OOP Limit Applies |
Blank, "Yes" or "No" |
35 |
Professional Services: Primary Care |
Cost sharing Type |
See note 1 |
36 |
Professional Services: Primary Care |
Benefit Deductible |
Blank or numeric |
37 |
Professional Services: Primary Care |
Co-payment |
Blank or numeric |
38 |
Professional Services: Primary Care |
Co-insurance |
Blank or numeric |
39 |
Professional Services: Primary Care |
Monthly Limits |
Blank, "None" or numeric |
40 |
Professional Services: Primary Care |
Annual Limits |
Blank, "None" or numeric |
41 |
Professional Services: Primary Care |
OOP Limit Applies |
Blank, "Yes" or "No" |
42 |
Professional Services: Emergency Department |
Cost sharing Type |
See note 1 |
43 |
Professional Services: Emergency Department |
Benefit Deductible |
Blank or numeric |
44 |
Professional Services: Emergency Department |
Co-payment |
Blank or numeric |
45 |
Professional Services: Emergency Department |
Co-insurance |
Blank or numeric |
46 |
Professional Services: Emergency Department |
Monthly Limits |
Blank, "None" or numeric |
47 |
Professional Services: Emergency Department |
Annual Limits |
Blank, "None" or numeric |
48 |
Professional Services: Emergency Department |
OOP Limit Applies |
Blank, "Yes" or "No" |
49 |
Professional Services: Specialist |
Cost sharing Type |
See note 1 |
50 |
Professional Services: Specialist |
Benefit Deductible |
Blank or numeric |
51 |
Professional Services: Specialist |
Co-payment |
Blank or numeric |
52 |
Professional Services: Specialist |
Co-insurance |
Blank or numeric |
53 |
Professional Services: Specialist |
Monthly Limits |
Blank, "None" or numeric |
54 |
Professional Services: Specialist |
Annual Limits |
Blank, "None" or numeric |
55 |
Professional Services: Specialist |
OOP Limit Applies |
Blank, "Yes" or "No" |
56 |
Professional Services: Obstetric Care (Bundled) |
Cost sharing Type |
See note 1 |
57 |
Professional Services: Obstetric Care (Bundled) |
Benefit Deductible |
Blank or numeric |
58 |
Professional Services: Obstetric Care (Bundled) |
Co-payment |
Blank or numeric |
59 |
Professional Services: Obstetric Care (Bundled) |
Co-insurance |
Blank or numeric |
60 |
Professional Services: Obstetric Care (Bundled) |
Monthly Limits |
Blank, "None" or numeric |
61 |
Professional Services: Obstetric Care (Bundled) |
Annual Limits |
Blank, "None" or numeric |
62 |
Professional Services: Obstetric Care (Bundled) |
OOP Limit Applies |
Blank, "Yes" or "No" |
63 |
Professional Services: Procedures & Other |
Cost sharing Type |
See note 1 |
64 |
Professional Services: Procedures & Other |
Benefit Deductible |
Blank or numeric |
65 |
Professional Services: Procedures & Other |
Co-payment |
Blank or numeric |
66 |
Professional Services: Procedures & Other |
Co-insurance |
Blank or numeric |
67 |
Professional Services: Procedures & Other |
Monthly Limits |
Blank, "None" or numeric |
68 |
Professional Services: Procedures & Other |
Annual Limits |
Blank, "None" or numeric |
69 |
Professional Services: Procedures & Other |
OOP Limit Applies |
Blank, "Yes" or "No" |
70 |
Professional Services: Physical Therapy |
Cost sharing Type |
See note 1 |
71 |
Professional Services: Physical Therapy |
Benefit Deductible |
Blank or numeric |
72 |
Professional Services: Physical Therapy |
Co-payment |
Blank or numeric |
73 |
Professional Services: Physical Therapy |
Co-insurance |
Blank or numeric |
74 |
Professional Services: Physical Therapy |
Monthly Limits |
Blank, "None" or numeric |
75 |
Professional Services: Physical Therapy |
Annual Limits |
Blank, "None" or numeric |
76 |
Professional Services: Physical Therapy |
OOP Limit Applies |
Blank, "Yes" or "No" |
77 |
Diagnostic Services: Radiology |
Cost sharing Type |
See note 1 |
78 |
Diagnostic Services: Radiology |
Benefit Deductible |
Blank or numeric |
79 |
Diagnostic Services: Radiology |
Co-payment |
Blank or numeric |
80 |
Diagnostic Services: Radiology |
Co-insurance |
Blank or numeric |
81 |
Diagnostic Services: Radiology |
Monthly Limits |
Blank, "None" or numeric |
82 |
Diagnostic Services: Radiology |
Annual Limits |
Blank, "None" or numeric |
83 |
Diagnostic Services: Radiology |
OOP Limit Applies |
Blank, "Yes" or "No" |
84 |
Diagnostic Services: Laboratory |
Cost sharing Type |
See note 1 |
85 |
Diagnostic Services: Laboratory |
Benefit Deductible |
Blank or numeric |
86 |
Diagnostic Services: Laboratory |
Co-payment |
Blank or numeric |
87 |
Diagnostic Services: Laboratory |
Co-insurance |
Blank or numeric |
88 |
Diagnostic Services: Laboratory |
Monthly Limits |
Blank, "None" or numeric |
89 |
Diagnostic Services: Laboratory |
Annual Limits |
Blank, "None" or numeric |
90 |
Diagnostic Services: Laboratory |
OOP Limit Applies |
Blank, "Yes" or "No" |
91 |
Prescription Drugs: Generic |
Cost sharing Type |
See note 1 |
92 |
Prescription Drugs: Generic |
Benefit Deductible |
Blank or numeric |
93 |
Prescription Drugs: Generic |
Co-payment |
Blank or numeric |
94 |
Prescription Drugs: Generic |
Co-insurance |
Blank or numeric |
95 |
Prescription Drugs: Generic |
Monthly Limits |
Blank, "None" or numeric |
96 |
Prescription Drugs: Generic |
Annual Limits |
Blank, "None" or numeric |
97 |
Prescription Drugs: Generic |
OOP Limit Applies |
Blank, "Yes" or "No" |
98 |
Prescription Drugs: Branded |
Cost sharing Type |
See note 1 |
99 |
Prescription Drugs: Branded |
Benefit Deductible |
Blank or numeric |
100 |
Prescription Drugs: Branded |
Co-payment |
Blank or numeric |
101 |
Prescription Drugs: Branded |
Co-insurance |
Blank or numeric |
102 |
Prescription Drugs: Branded |
Monthly Limits |
Blank, "None" or numeric |
103 |
Prescription Drugs: Branded |
Annual Limits |
Blank, "None" or numeric |
104 |
Prescription Drugs: Branded |
OOP Limit Applies |
Blank, "Yes" or "No" |
105 |
Over-the-counter Drugs |
Cost sharing Type |
See note 1 |
106 |
Over-the-counter Drugs |
Benefit Deductible |
Blank or numeric |
107 |
Over-the-counter Drugs |
Co-payment |
Blank or numeric |
108 |
Over-the-counter Drugs |
Co-insurance |
Blank or numeric |
109 |
Over-the-counter Drugs |
Monthly Limits |
Blank, "None" or numeric |
110 |
Over-the-counter Drugs |
Annual Limits |
Blank, "None" or numeric |
111 |
Over-the-counter Drugs |
OOP Limit Applies |
Blank, "Yes" or "No" |
112 |
Preventive Services & Vaccines |
Cost sharing Type |
See note 1 |
113 |
Preventive Services & Vaccines |
Benefit Deductible |
Blank or numeric |
114 |
Preventive Services & Vaccines |
Co-payment |
Blank or numeric |
115 |
Preventive Services & Vaccines |
Co-insurance |
Blank or numeric |
116 |
Preventive Services & Vaccines |
Monthly Limits |
Blank, "None" or numeric |
117 |
Preventive Services & Vaccines |
Annual Limits |
Blank, "None" or numeric |
118 |
Preventive Services & Vaccines |
OOP Limit Applies |
Blank, "Yes" or "No" |
119 |
Durable Medical Equipment |
Cost sharing Type |
See note 1 |
120 |
Durable Medical Equipment |
Benefit Deductible |
Blank or numeric |
121 |
Durable Medical Equipment |
Co-payment |
Blank or numeric |
122 |
Durable Medical Equipment |
Co-insurance |
Blank or numeric |
123 |
Durable Medical Equipment |
Monthly Limits |
Blank, "None" or numeric |
124 |
Durable Medical Equipment |
Annual Limits |
Blank, "None" or numeric |
125 |
Durable Medical Equipment |
OOP Limit Applies |
Blank, "Yes" or "No" |
126 |
Medical Supplies |
Cost sharing Type |
See note 1 |
127 |
Medical Supplies |
Benefit Deductible |
Blank or numeric |
128 |
Medical Supplies |
Co-payment |
Blank or numeric |
129 |
Medical Supplies |
Co-insurance |
Blank or numeric |
130 |
Medical Supplies |
Monthly Limits |
Blank, "None" or numeric |
131 |
Medical Supplies |
Annual Limits |
Blank, "None" or numeric |
132 |
Medical Supplies |
OOP Limit Applies |
Blank, "Yes" or "No" |
133 |
Over-the-counter Medical Supplies |
Cost sharing Type |
See note 1 |
134 |
Over-the-counter Medical Supplies |
Benefit Deductible |
Blank or numeric |
135 |
Over-the-counter Medical Supplies |
Co-payment |
Blank or numeric |
136 |
Over-the-counter Medical Supplies |
Co-insurance |
Blank or numeric |
137 |
Over-the-counter Medical Supplies |
Monthly Limits |
Blank, "None" or numeric |
138 |
Over-the-counter Medical Supplies |
Annual Limits |
Blank, "None" or numeric |
139 |
Over-the-counter Medical Supplies |
OOP Limit Applies |
Blank, "Yes" or "No" |
140 |
Other Items & Services |
Cost sharing Type |
See note 1 |
141 |
Other Items & Services |
Benefit Deductible |
Blank or numeric |
142 |
Other Items & Services |
Co-payment |
Blank or numeric |
143 |
Other Items & Services |
Co-insurance |
Blank or numeric |
144 |
Other Items & Services |
Monthly Limits |
Blank, "None" or numeric |
145 |
Other Items & Services |
Annual Limits |
Blank, "None" or numeric |
146 |
Other Items & Services |
OOP Limit Applies |
Blank, "Yes" or "No" |
Note 1: One of the 19 cost sharing options listed in §4.2, Table 4.2. Must match the spelling of one of the 19 options.
Appendix C: PLAN_OUTPUT_DATA external data file
The CECSC generates an external data file containing the output data for the plans listed in the PLAN_INPUT_DATA worksheet. (NOTE: when the CECSC generates output data it also generates a corresponding PLAN_INPUT_DATA file. Therefore be careful not to overwrite an input data file.)
The CECSC output data file consists of a tab-separated text file containing 19 variables. These correspond to the data that are generated and stored on the PLAN_OUTPUT_DATA worksheet. The outputs from the CECSC can be used to populate the Deductibles, Copayments, Coinsurance, Limits or Exclusions, and Total [patient] would pay is sections of the coverage example in the SBC.
The plan identifier (PLAN_ID)
Six output variables for the Maternity example:
The amount of the plan payment
The amount of the subscriber payment
The amount of the subscriber payment attributable to deductibles
The amount of the subscriber payment attributable to co-payment
The amount of the subscriber payment attributable to co-insurance
The amount of the subscriber payment attributable to exclusions and non-covered items and services
Six output variables for the Diabetes example:
The amount of the plan payment
The amount of the subscriber payment
The amount of the subscriber payment attributable to deductibles
The amount of the subscriber payment attributable to co-payment
The amount of the subscriber payment attributable to co-insurance
The amount of the subscriber payment attributable to exclusions and non-covered items and services
Six output variables for the Foot Fracture example:
The amount of the plan payment
The amount of the subscriber payment
The amount of the subscriber payment attributable to deductibles
The amount of the subscriber payment attributable to co-payment
The amount of the subscriber payment attributable to co-insurance
The amount of the subscriber payment attributable to exclusions and non-covered items and services
1 The “allowed amount” is the maximum amount that the plan will pay for the item or service. Technically, a non-covered service would not have an “allowed amount”, and the subscriber’s out-of-pocket payment would be whatever the provider or supplier of the item or service charges.
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| File Title | Coverage Examples Cost Sharing Calculator |
| Author | Henry Bachofer |
| File Modified | 0000-00-00 |
| File Created | 2021-01-15 |
© 2026 OMB.report | Privacy Policy