CMS-10668 CDI Validation Template
Quality Measures and Administrative Procedures for the Hospital-Acquired Condition Reduction Program for the FY 2019 IPPS Program Year (CMS-10668)
FY2021_CDI_Validation Template_4.12.2018.FINAL(508).xlsx
Hospital-Acquired Condition Reduction Program-NHSN HAI Measures Validation
OMB: 0938-1352
⚠️ Notice: This form may be outdated. More recent filings and information on OMB 0938-1352 can be found here:
Document [xlsx]
Download: xlsx | pdf
Template
NHSN Location
FY2021 Submission Instructions
Overview
DefinitionsTemplate
NHSN Location
FY2021 Submission Instructions
Sheet 1: Definitions
| Clostridium Difficile Infection (CDI) Validation Template |
||
| In support of validation of laboratory-identified CDI events reported for the Hospital Inpatient Quality Reporting (IQR) Program for the Fiscal Year (FY) 2021 | ||
| payment determination: | ||
| • Each hospital selected for CDI validation is to produce a list of all final results for stool specimens that are toxin positive for CDI during an inpatient | ||
| episode of care. | ||
| • The list may include specimens collected in the ED and/or 24-hour observation locations collected prior to an inpatient admission; however, if the patient | ||
| was only seen in the ED and/or 24-hour observation and never admitted to an inpatient location, do not include these on the Validation Template. These are | ||
| scenarios where the Centers for Medicare and Medicaid Services (CMS) and the National Healthcare Safety Network (NHSN) reporting differ. | ||
| • The line list should include stool specimens that are toxin positive for CDI from unformed stools only. | ||
| Exclusions include: C-diff antigen positive, antigen only detected, no toxin detected | ||
| FY 2021 - CDI Validation Template | ||
| (Use this template for stool specimens toxin positive for CDI beginning with 3Q18 - all quarters must be submitted on separate templates) | ||
| FIELD (* indicates required field) | DESCRIPTION | SECTION |
| NHSN Facility ID* | The National Healthcare Safety Network (NHSN)-assigned facility ID under which your hospital submits NHSN data. | 
|
| Provider ID/CCN* | Hospital's 6-digit CMS Certification Number (CCN). | |
| Hospital Name* | Hospital Name associated with CCN. | |
| State* | Enter the 2 character abbreviation for the state in which the hospital is located. | |
| Calendar Quarter* | Select from the drop-down list the calendar quarter to which the CDI Validation Template pertains. | |
| Hospital Contact Name* | Hospital contact name for CMS to contact with questions. | |
| Contact Phone* | Phone number for hospital contact listed. | |
| Contact Email* | Email address for hospital contact listed. | |
| Assay Type* | The type of test used to detect CDI. | |
| Stool Specimens Toxin Positive for C. difficile (Y/N)* | Select Yes or No from the drop-down list. Does the hospital have any final stool cultures toxin positive for CDI for patients in the calendar quarter referenced? | |
| Patient Identifier* | The patient identifier assigned by the hospital. Use the same patient identifier that would be submitted to NHSN if the episode of care (EOC) would be reported as a laboratory-identified CDI event. | |
| Birthdate* | The patient date of birth using MM/DD/YYYY format. | |
| Sex* | Select Female, Male or unknown from the drop-down list to indicate the sex of patient. | 
|
| Admit Date* | Enter date patient was admitted to hospital in MM/DD/YYYY format. | |
| Discharge Date* | Enter date patient was discharged from the hospital in MM/DD/YYYY format. If a patient has not been discharged from the hospital enter "Not Discharged" for the Discharge Date field. | |
| First Name | First name of patient. | |
| Last Name | Last name of patient. | |
| NHSN Location* | Select from the drop-down list, the NHSN location to which the patient was assigned when the stool specimen was collected. Only locations from the drop-down will be accepted; do not use a hospital-assigned location. |
|
| Lab ID* | Lab ID, accession number or specimen number corresponding to toxin positive for CDI stool specimen. | |
| Stool Specimen Collection Date* | Provide the date the stool specimen was collected in MM/DD/YYYY format. | |
| Stool Specimen Collection Time | Provide the time the stool specimen was collected if easily available. | |
| Blank cell | ||
| For additional information, view the appropriate CDI Abstraction Manual posted on the Inpatient Chart-Abstracted Data Validation page of QualityNet. | ||
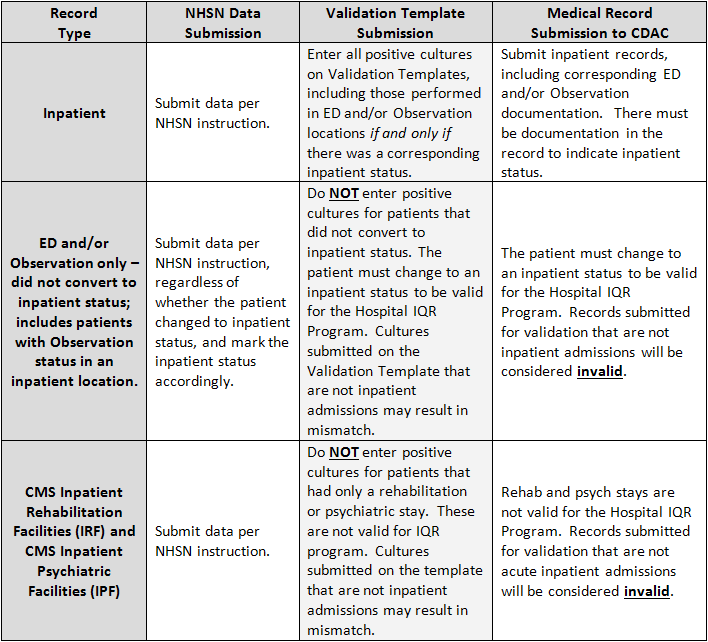
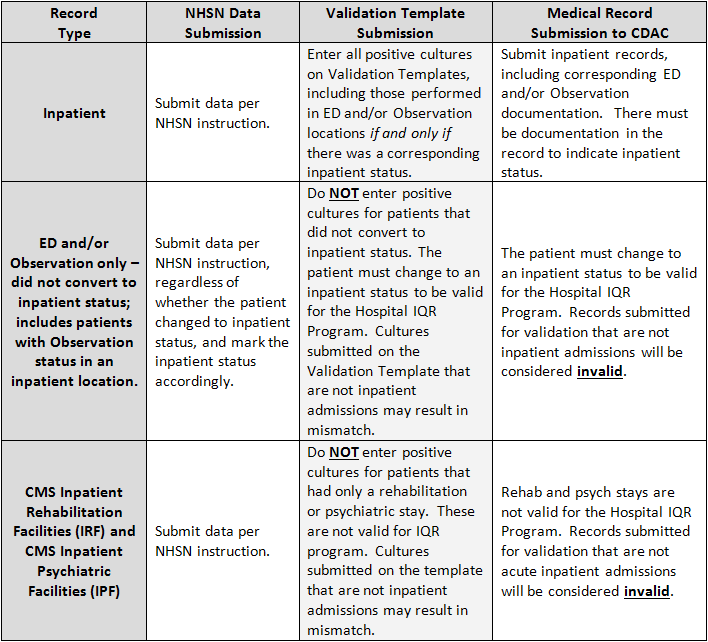
| For the purposes of Hospital IQR Program Chart-Abstracted Data Validation, please note the differences between NHSN data submission | ||
| and validation template/medical record submission, as described below: | ||
| End of worksheet | ||
| PRA Disclosure Statement According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is 0938-XXXX (Expires XX/XX/XXXX). The time required to complete this information collection is estimated to average 8 hours per response, including the time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection. If you have comments concerning the accuracy of the time estimate(s) or suggestions for improving this form, please write to CMS, 7500 Security Boulevard, Attn: PRA Reports Clearance Officer, Mail Stop C4-26-05, Baltimore, Maryland 21244-1850. ****CMS Disclosure**** Please do not send applications, claims, payments, medical records or any documents containing sensitive information to the PRA Reports Clearance Office. Please note that any correspondence not pertaining to the information collection burden approved under the associated OMB control number listed on this form will not be reviewed, forwarded, or retained. If you have questions or concerns regarding where to submit your documents, please contact validation@hcqis.org. |
||
Sheet 2: Template
| NHSN Facility ID* | Provider ID/CCN* | Hospital Name* | State* | Calendar Quarter* | Hospital Contact Name* | Contact Phone* | Contact Email* | Assay Type* | Stool Specimens Toxin Positive for C. difficile (Y/N)* | Patient Identifier* | Birthdate* | Sex* | Admit Date* | Discharge Date* | First Name | Last Name | NHSN Location* | Lab ID* | Stool Specimen Collection Date* | Stool Specimen Collection Time |
Sheet 3: NHSN Location
| NHSN Locations Included in the Hospital IQR Program's CDI Reporting | ||
| CDC LOCATION LABEL | LOCATION DESCRIPTION | CDC LOCATION CODE |
| Inpatient Adult Critical Care Units | ||
| Burn Critical Care | Critical care area specializing in the care of patients with significant/major burns. | IN:ACUTE:CC:B |
| Medical Cardiac Critical Care | Critical care area specializing in the care of patients with serious heart problems that do not require heart surgery. | IN:ACUTE:CC:C |
| Medical Critical Care | Critical care area for patients who are being treated for nonsurgical conditions. | IN:ACUTE:CC:M |
| Medical/Surgical Critical Care | An area where critically ill patients with medical and/or surgical conditions are managed. | IN:ACUTE:CC:MS |
| Neurologic Critical Care | Critical care area for the care of patients with life-threatening neurologic diseases. | IN:ACUTE:CC:N |
| Neurosurgical Critical Care | Critical care area for the surgical management of patients with severe neurologic diseases or those at risk for neurologic injury as a result of surgery. | IN:ACUTE:CC:NS |
| ONC Medical Critical Care | Critical care area for the care of oncology patients who are being treated for nonsurgical conditions related to their malignancy. | IN:ACUTE:CC:ONC_M |
| ONC Surgical Critical Care | Critical care area for the evaluation and management of oncology patients with serious illness before and/or after cancer-related surgery. | IN:ACUTE:CC:ONC_S |
| ONC Medical-Surgical Critical Care | Critical care area for the care of oncology patients with medical and/or surgical conditions related to their malignancy. | IN:ACUTE:CC:ONC_MS |
| Prenatal Critical Care | Critical care area for the care of pregnant patients with complex medical or obstetric problems requiring a high level of care to prevent the loss of the fetus and to protect the life of the mother. | IN:ACUTE:CC:PNATL |
| Respiratory Critical Care | Critical care area for the evaluation and treatment of patients with severe respiratory conditions. | IN:ACUTE:CC:R |
| Surgical Cardiothoracic Critical Care | Critical care area specializing in the care of patients following cardiac and thoracic surgery. | IN:ACUTE:CC:CT |
| Surgical Critical Care | Critical care area for the evaluation and management of patients with serious illness before and/or after surgery. | IN:ACUTE:CC:S |
| Trauma Critical Care | Critical care area specializing in the care of patients who require a high level of monitoring and/or intervention following trauma or during critical illness related to trauma. | IN:ACUTE:CC:T |
| Inpatient Pediatric Critical Care Units | ||
| ONC Pediatric Critical Care | Critical care area for the care of oncology patients ≤18 years old who are being treated for surgical or nonsurgical conditions related to their malignancy. | IN:ACUTE:CC:ONC_PED |
| Pediatric Burn Critical Care | Critical care area specializing in the care of patients ≤ 18 years old with significant/major burns. | IN:ACUTE:CC:B_PED |
| Pediatric Cardiothoracic Critical Care | Critical care area specializing in the care of patients ≤ 18 years old following cardiac and thoracic surgery. | IN:ACUTE:CC:CT_PED |
| Pediatric Medical Critical Care | Critical care area for patients ≤ 18 years old who are being treated for nonsurgical conditions. In the NNIS system, this was called Pediatric ICU (PICU). | IN:ACUTE:CC:M_PED |
| Pediatric Medical Surgical Critical Care | An area where critically ill patients ≤ 18 years old with medical and/or surgical conditions are managed. | IN:ACUTE:CC:MS_PED |
| Pediatric Neurosurgical Critical Care | Critical care area specializing in the surgical management of patients ≤ 18 years old with severe neurological diseases or those at risk for neurological injury as a result of surgery. | IN:ACUTE:CC:NS_PED |
| Pediatric Respiratory Critical Care | Critical care area for the evaluation and treatment of the patients ≤ 18 years old with severe respiratory conditions. | IN:ACUTE:CC:R_PED |
| Pediatric Surgical Critical Care | Critical care area for the evaluation and management of patients ≤ 18 years old with serious illness before and/or after surgery. | IN:ACUTE:CC:S_PED |
| Pediatric Trauma Critical Care | Critical care area specializing in the care of patients ≤ 18 years old who require a high level of monitoring and/or intervention following trauma or during critical illness related to trauma. | IN:ACUTE:CC:T_PED |
| Inpatient Neonatal Units | ||
| Well Baby Nursery (Level I) | Hospital area for evaluation and postnatal care of healthy newborns. May include neonatal resuscitation and stabilization of ill newborns until transfer to a facility at which specialty neonatal care is provided. | IN:ACUTE:WARD:NURS |
| Step down Neonatal Nursery (Level II) | NOTE: The categories of Level II, listed below, are classifications from the American Academy of Pediatrics, Definitions of hospital-based newborn services. Level II neonatal care (specialty) Special care nursery: level II units are subdivided into 2 categories on the basis of their ability to provide assisted ventilation including continuous positive airway pressure. Level IIA: has the capabilities to • Resuscitate and stabilize preterm and/or ill infants before transfer to a facility at which newborn intensive care is provided. • Provide care for infants born at >32 weeks’ gestation and weighing ≥1500 g (1) who have physiologic immaturity such as apnea of prematurity, inability to maintain body temperature, or inability to take oral feedings or (2) who are moderately ill with problems that are anticipated to resolve rapidly and are not anticipated to need subspecialty services on an urgent basis. • Provide care for infants who are convalescing after intensive care. Level IIB has the capabilities of a level IIA nursery and the additional capability to provide mechanical ventilation for brief durations (<24 hours) or continuous positive airway pressure. |
IN:ACUTE:STEP:NURS |
| Neonatal Critical Care Level II/III | Combined nursery housing both Level II and III newborns and infants. | IN:ACUTE:CC_STEP:NURS |
| Neonatal Critical Care Level III | A hospital neonatal intensive care unit (NICU) organized with personnel and equipment to provide continuous life support and comprehensive care for extremely high-risk newborn infants and those with complex and critical illness. NOTE: The categories of Level III below are classifications from the American Academy of Pediatrics, Definitions of hospital-based newborn services.1 These classifications are all considered Level III nurseries in NHSN. Level III (subspecialty) NICU: level III NICUs are subdivided into 3 categories: Level IIIA: has the capabilities to • Provide comprehensive care for infants born at >28 weeks’ gestation and weighing >1000 g. • Provide sustained life support limited to conventional mechanical ventilation. • Perform minor surgical procedures such as placement of central venous catheter or inguinal hernia repair Level IIIB NICU: has the capabilities to provide. • Comprehensive care for extremely low birth weight infants (≤1000 g and ≤28 weeks’ gestation). • Advanced respiratory support such as high-frequency ventilation and inhaled nitric oxide for as long as required. • Prompt and on-site access to a full range of pediatric medical subspecialists. • Advanced imaging, with interpretation on an urgent basis, including computed tomography, magnetic resonance imaging, and echocardiography. • Pediatric surgical specialists and pediatric anesthesiologists on site or at a closely related institution to perform major surgery such as ligation of patent ductus arteriosus and repair of abdominal wall defects, necrotizing enterocolitis with bowel perforation, tracheoesophageal fistula and/or esophageal atresia, and myelomeningocele. Level IIIC NICU has the capabilities of a level IIIB NICU and also is located within an institution that has the capability to provide ECMO and surgical repair of complex congenital cardiac malformations that require cardiopulmonary bypass. |
IN:ACUTE:CC:NURS |
| Inpatient Specialty Care Areas (SCA) | ||
| Inpatient Dialysis SCA | Hospital specialty care area for patients who require dialysis as part of their care. These patients may be chronic or acute dialysis patients. | IN:ACUTE:SCA:DIAL |
| Pediatric Dialysis SCA | Hospital specialty care area for patients ≤18 years old who require acute dialysis as part of their care. These patients may be chronic or acute dialysis patients. | IN:ACUTE:SCA:DIAL_PED |
| Pediatric Solid Organ Transplant SCA | Hospital specialty area for the postoperative care of patients ≤18 years old who have had a solid organ transplant (e.g., heart/lung, kidney, liver, pancreas). | IN:ACUTE:SCA:SOTP_PED |
| Solid Organ Transplant SCA | Hospital specialty area for the postoperative care of patients who have had a solid organ transplant (e.g., heart/lung, kidney, liver, pancreas). | IN:ACUTE:SCA:SOTP |
| Inpatient Adult Wards | ||
| Antenatal Care Ward | Hospital area for observation, evaluation, treatment or surgery of high risk pregnancy patients. | IN:ACUTE:WARD: ANTENAT |
| Behavioral Health /Psych Ward | Area for the evaluation and treatment of patients with acute psychiatric or behavioral disorders. | IN:ACUTE:WARD:BHV |
| Burn Ward | Hospital area for evaluation and treatment of patients who have burns. | IN:ACUTE:WARD:B |
| Ear/Nose/Throat Ward | Hospital area for the evaluation, treatment, or surgery of patients with ear, nose, or throat disorders. | IN:ACUTE:WARD:ENT |
| Gastrointestinal Ward | Hospital area for evaluation, treatment or surgery of patients with disorders of the gastrointestinal tract. | IN:ACUTE:WARD:GI |
| Genitourinary Ward | Hospital area for the evaluation, treatment or surgery of patients with disorders of the genitourinary system. | IN:ACUTE:WARD:GU |
| Gerontology Ward | Hospital area for the evaluation, treatment or surgery of patients with age-related diseases. | IN:ACUTE:WARD:GNT |
| Gynecology Ward | Hospital area for the evaluation, treatment, or surgery of female patients with reproductive tract disorders. | IN:ACUTE:WARD:GYN |
| Jail Unit* | Overnight stay patient care area of a hospital or correctional facility used only for those who are in custody of law enforcement during their treatment. | IN:ACUTE:WARD:JAL |
| Labor and Delivery Ward | Hospital area where women labor and give birth. | IN:ACUTE:WARD:LD |
| Labor, Delivery, Recovery, Postpartum Suite (LDRP) | Hospital suite used for labor, delivery, recovery and post-partum (LDRP) -- all within the same suite. | IN:ACUTE:WARD:LD_PP |
| Medical Ward | Hospital area for the evaluation and treatment of patients with medical conditions or disorders. | IN:ACUTE:WARD:M |
| Medical/Surgical Ward | Hospital area for the evaluation of patients with medical and/or surgical conditions. | IN:ACUTE:WARD:MS |
| Neurology Ward | Hospital area where patients with neurological disorders are evaluated and treated. | IN:ACUTE:WARD:N |
| Neurosurgical Ward | Hospital area for care of patients whose primary reason for admission is to have neurosurgery or to be cared for by a neurosurgeon after head or spinal trauma. | IN:ACUTE:WARD:NS |
| ONC Leukemia Ward | Area for the evaluation and treatment of patients with leukemia. | IN:ACUTE:WARD:ONC_LEUK |
| ONC Lymphoma Ward | Area for the evaluation and treatment of patients with lymphoma. | IN:ACUTE:WARD:ONC:LYMPH |
| ONC Leukemia/Lymphoma Ward | Area for the evaluation and treatment of patients with leukemia and/or lymphoma. | IN:ACUTE:WARD: ONC_LL |
| ONC Solid Tumor Ward | Area for the evaluation and treatment of oncology patients with solid tumors. | IN:ACUTE:WARD:ONC_ST |
| ONC Hematopoietic Stem Cell Transplant Ward | Area for the care of patients who undergo stem cell transplant for the treatment of cancers and/or blood or immune system disorders. | IN:ACUTE:WARD: ONC_HSCT |
| ONC General Hematology/Oncology Ward | Area for the evaluation and treatment of patients with cancer and/or blood disorders. | IN:ACUTE:WARD: ONC_HONC |
| Ophthalmology Ward | Hospital area for care of patients whose primary reason for admission is to have eye surgery or to be cared for by an ophthalmologist after eye trauma. | IN:ACUTE:WARD:OPH |
| Orthopedic Ward | Hospital area for evaluation, treatment or surgery on bones, joints, and associated structures by an orthopedist. | IN:ACUTE:WARD:ORT |
| Orthopedic Trauma Ward | Hospital area where patients with orthopedic injuries or disorders are evaluated and treated. | IN:ACUTE:WARD_ORT |
| Plastic Surgery Ward | Hospital area for the care of patients who have reconstructive surgery performed by a plastic surgeon. | IN:ACUTE:WARD:PLS |
| Postpartum Ward | Hospital area for the patient who is recovering from childbirth. | IN:ACUTE:WARD:PP |
| Pulmonary Ward | Hospital area where patients with respiratory system conditions or disorders are evaluated and treated. | IN:ACUTE:WARD:PULM |
| Rehabilitation Ward | Hospital area for evaluation and restoration of function to patients who have lost function due to acute or chronic pain, musculoskeletal problems, stroke, or catastrophic events resulting in complete or partial paralysis. | IN:ACUTE:WARD:REHAB |
| School Infirmary* | Overnight stay patient care area of a school infirmary or health center (e.g., private residential school or college campus). | IN:ACUTE:WARD:IFM |
| Stroke (Acute) Ward | Hospital area for evaluation, stabilization and treatment of patients who have experienced an acute stroke. | IN:ACUTE:WARD:STRK |
| Surgical Ward | Hospital area for evaluation and treatment of patients who have undergone a surgical procedure. | IN:ACUTE:WARD:S |
| Telemetry Ward | Hospital area dedicated to providing evaluation and treatment of patients requiring continuous cardiac monitoring. | IN:ACUTE:WARD:TEL |
| Vascular Surgery Ward | Hospital area for evaluation and treatment of patients who have undergone vascular surgery. | IN:ACUTE:WARD:VS |
| Inpatient Pediatric Wards | ||
| Adolescent Behavioral Health Ward | Hospital area for evaluation and treatment of patients between the ages of 13 and 18 with acute psychiatric or behavioral disorders. | IN:ACUTE:WARD: BHV_ADOL |
| ONC Pediatric Hematopoietic Stem Cell Transplant Ward | Area for the care of patients ≤18 years old who undergo stem cell transplant for the treatment of cancers and/or blood or immune system disorders. | IN:ACUTE:WARD:ONC_HSCT_PED |
| ONC Pediatric General Hematology/Oncology Ward | Area for the evaluation and treatment of patients ≤18 years old with cancer and/or blood disorders. | IN:ACUTE:WARD:ONC_HONC_PED |
| Pediatric Behavioral Health Ward | Hospital area for evaluation and management of patients ≤18 years old with acute psychiatric or behavioral disorders. | IN:ACUTE:WARD:BHV_PED |
| Pediatric Burn Ward | Hospital area specializing in the evaluation and treatment of patients ≤18 years old who have tissue injury caused by burns. | IN:ACUTE:WARD:B_PED |
| Pediatric Ear, Nose, Throat Ward | Hospital area for evaluation and management of patients ≤18 years old with disorders of the ear, nose and/or throat. | IN:ACUTE:WARD: ENT_PED |
| Pediatric Genitourinary Ward | Hospital area where patients ≤18 years old with disorders of the genitourinary system are evaluated and treated. | IN:ACUTE:WARD: GU_PED |
| Pediatric Medical Ward | Area for the evaluation and treatment of patients ≤18 years of old with medical conditions or disorders. | IN:ACUTE:WARD:M_PED |
| Pediatric Medical/Surgical Ward | Hospital area where patients ≤18 years old with medical and/or surgical conditions are managed. | IN:ACUTE:WARD: MS_PED |
| Pediatric Neurology Ward | Area for the evaluation and treatment of patients ≤18 years old with neurologic disorders. | IN:ACUTE:WARD:N_PED |
| Pediatric Neurosurgical Ward | Hospital area for care of patients ≤18 years old whose primary reason for admission is to have neurosurgery or to be cared for by a neurosurgeon after head or spinal trauma. | IN:ACUTE:WARD:NS_PED |
| Pediatric Orthopedic Ward | Hospital area where patients ≤18 years old with orthopedic injuries or disorders are evaluated and treated. | IN:ACUTE:WARD:ORT_PED |
| Pediatric Rehabilitation Ward | Hospital area for evaluation and restoration of function to patients ≤18 years old who have lost function due to acute or chronic pain, musculoskeletal problems, stroke, or catastrophic events resulting in complete or partial paralysis. | IN:ACUTE:WARD:REHAB_PED |
| Pediatric Surgical Ward | Hospital area for evaluation and treatment of patients ≤18 years old that have undergone a surgical procedure. | IN:ACUTE:WARD:S_PED |
| Inpatient Step Down Units | ||
| Adult Step Down Unit (e.g., post-critical care) | Hospital area for adult patients that are hemodynamically stable who can benefit from close supervision and monitoring, such as frequent pulmonary toilet, vital signs, and/or neurological and neurovascular checks. | IN:ACUTE:STEP |
| ONC Step Down Unit (all ages) (e.g., post-critical care) | Area for oncology patients who are hemodynamically stable and can benefit from close supervision and monitoring, such as frequent pulmonary toilet, vital signs, and/or neurologic and neurovascular checks. | IN:ACUTE:STEP:ONC |
| Pediatric Step Down Unit (e.g., post-critical care) | Patients ≤18 years old that are hemodynamically stable who can benefit from close supervision and monitoring, such as frequent pulmonary toilet, vital signs, and/or neurological and neurovascular checks. | IN:ACUTE:STEP:PED |
| Inpatient Mixed Acuity Units | ||
| Adult Mixed Acuity Unit | Hospital area for the evaluation and treatment of adult patients whose conditions are varying levels of acuity (e.g., critical care, ward-level care, step-down type care, etc.). Such a care area may be comprised of patients followed by different hospital services (e.g., coronary, medical, surgical, etc.). This care area may or may not include “acuity adaptable” or “universal” beds (i.e., this model of patient care allows a patient to stay in the same bed during all phases of his care, from critical care through lower levels of care). | IN:ACUTE:MIXED:ALL_ADULT |
| Pediatric Mixed Acuity Unit | Hospital area for the evaluation and treatment of pediatric patients (≤18 years old) whose conditions are of varying levels of acuity (e.g., critical care, etc.). Such a care area may be comprised of patients followed by different hospital services (e.g., coronary, medical, surgical, etc.). This care area may or may not include “acuity adaptable” or “universal” beds (i.e., this model of patient care allows a patient to stay in the same bed during all phases of his care, from critical care through lower levels of care). | IN:ACUTE:MIXED: ALL_PEDS |
| Mixed Age Mixed Acuity Unit | Hospital area for the evaluation and treatment of a mixture of adult and pediatric patients whose conditions are of varying levels of acuity (e.g., critical care, ward-level care, step-down type care, etc.). Such a care area may be comprised of patients followed by different hospital services (e.g., coronary, medical, surgical, etc.). This care area may or may not include “acuity adaptable” or “universal” beds (i.e., this model of patient care allows a patient to stay in the same bed during all phases of his care, from critical care through lower levels of care). | IN:ACUTE:MIXED:ALL |
| ONC Mixed Acuity Unit (all ages) |
Area for the evaluation and treatment of a mixture of adult and pediatric oncology patients whose conditions are of varying levels of acuity (e.g., critical care, ward-level care, step down type care, etc.). This care area may or may not include ''acuity adaptable'' or ''universal'' beds (i.e., this model of patient care allows a patient to stay in same bed during all phases of care, from critical care through lower levels of care). | IN:ACUTE:MIXED:ONC |
| Inpatient Operating Rooms | ||
| Cardiac Catheterization Room/Suite | A room or rooms in a hospital equipped for the performance of heart catheterizations for diagnostic or therapeutic purposes. Operating Room requirements for air changes, temperature, humidity and surfaces must be met. | IN:ACUTE:OR:CATH |
| Cesarean Section Room/Suite | A room or suite in a hospital equipped for the performance of obstetric and gynecologic surgeries and for the care of the neonate immediately after birth. Operating Room requirements for air changes, temperature, humidity and surfaces must be met. | IN:ACUTE:OR:LD |
| Interventional Radiology | A room or suite in a hospital where diagnostic or therapeutic radiologic procedures on outpatients and/or inpatients occurs. Operating Room requirements for air changes, temperature, humidity and surfaces must be met. | IN:ACUTE:OR:RAD |
| Operating Room/Suite | A room or suite in a hospital equipped for the performance of surgical operations. Requirements for air changes, temperature, humidity and surfaces must be met. (For outpatient operating room, use Ambulatory Surgery Center designation or other specialty OR shown in Outpatient Locations section of this chapter). | IN:ACUTE:OR |
| Post Anesthesia Care Unit/Recovery Room | Hospital area designated for monitoring patients for immediate effects of anesthesia before either going home or on to an in-patient care area. | IN:ACUTE:OR_STEP |
| Inpatient Chronic Care Units | ||
| Inpatient Hospice* | Area where palliative care is provided to the terminally ill patient. | IN:NONACUTE:LTC:HSP |
| Chronic Alzheimer's Unit* | Area where care is provided to patients diagnosed with Alzheimer's syndrome for extended periods of time. Formerly called Long Term Care Alzheimer’s Unit. | IN:NONACUTE:LTC:ALZ |
| Chronic Behavioral Health/Psych Unit* | Area where care is provided to patients with psychiatric or behavioral-disorder diagnoses for extended periods of time. Formerly called Long Term Care Behavioral Health/Psych Unit. | IN:NONACUTE:LTC:BHV |
| Chronic Rehabilitation Unit* | Area where evaluation and restoration of function is provided to patients who have lost function due to acute or chronic pain, musculoskeletal problems, stroke, or catastrophic events resulting in complete or partial paralysis. Formerly called Long Term Care Rehabilitation Unit. | IN:NONACUTE:LTC: REHAB |
| Chronic Care Unit* | Area where care provided for patients with chronic disease or disabilities for extended periods of time. Formerly called Long Term Care Unit. | IN:NONACUTE:LTC |
| Ventilator Dependent Unit* | Area where care is provided to patients whose respirations depend on the use of a ventilator for extended periods of time. | IN:NONACUTE:LTC:R |
| Acute Care Facilities General | ||
| 24-Hour Observation Area | Area where patients are monitored for suspected or non-life threatening conditions for 24 hours or less. More than 50% of patients in this location must be outpatients who are not expected to be admitted to an inpatient unit. | OUT:ACUTE:WARD |
| Ambulatory Surgery Center | Area that is equipped for the performance of surgical operations; may be free-standing or part of a hospital. Operating Room requirements for air changes, temperature, humidity and surfaces must be met. | OUT:ACUTE:OR |
| Emergency Department | Area that provides emergency medical services; top priority is given to those with life-threatening illness or injury. | OUT:ACUTE:ED |
| Mobile Emergency Services/EMS | Mobile unit that provides clinical and emergency medical services to patients who require them in the pre-hospital setting. | OUT:ACUTE:MOBILE:UE |
| Ambulatory Pediatric Surgery Center | Area that is equipped for the performance of surgical operations for patients ≤18 years old; may be free-standing or part of a hospital. Operating Room requirements for air changes, temperature, humidity and surfaces must be met. | OUT:ACUTE:OR:PED |
| Ambulatory Plastic Surgery Center | Area that is equipped for the performance of plastic surgery operations; may be free-standing or part of a hospital. Operating Room requirements for air changes, temperature, humidity and surfaces must be met. | OUT:ACUTE:OR:PLS |
| Ambulatory Surgery Recovery Room/Post Anesthesia Care Unit | Area designated for monitoring patients for the immediate effects of anesthesia before being sent home. | OUT:ACUTE:OR_STEP |
| Pediatric Emergency Department | Area that provides emergency medical services to patients ≤18 years old; top priority is given to those with life-threatening illness or injury. | OUT:ACUTE:ED:PED |
| Urgent Care Center | Area that provides medical care services for illnesses and injuries that are not life-threatening. | OUT:ACUTE:CLINIC:UE |
| Facility-Wide Locations | ||
| Facility-wide Inpatient FacWideIN | This location represents all inpatient locations for the facility, where appropriate numerator and denominator counts can be collected. All of the facility’s inpatient locations with an overnight stay must be represented for full inpatient facility coverage, where denominators can be accurately collected and there is the possibility of the MDRO to present, transmitted, and identified in that specific location. Currently, it is available for use in the MDRO/CDI Module for LabID Event reporting and in the AUR Module. | FACWIDEIN |
| Facility-wide Outpatient FacWideOUT | This location represents all outpatient locations for the facility, where appropriate numerator and accurate denominator counts can be collected. All of the facility’s outpatient locations must be represented for full outpatient facility coverage, where denominators can be accurately collected and there is the possibility of the MDRO to be present, transmitted, and identified in that specific location. Currently, it is available for use in the MDRO/CDI Module for LabID Event reporting. | FACWIDEOUT |
| * Include only inpatient episodes of care billed under the hospital’s acute care CMS certification number (regardless of payer) |
Sheet 4: FY2021 Submission Instructions
| USER GUIDE AND SUBMISSION INSTRUCTIONS | ||||||||||||||||
| ---> | The FY 2021 Validation Template User Guide and Submission Instructions, along with supporting documentation, can be found on QualityNet by hovering | |||||||||||||||
| over the Hospitals - Inpatient drop-down and selecting the [Data Validation (Chart-Abstracted & eCQM)] link, followed by selecting the | ||||||||||||||||
| [Chart-Abstracted Data Validation] program. From the navigation bar on the left side of the Chart-Abstracted Data Validation Overview page, select [Resources]: | ||||||||||||||||
| https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier4&cid=1140537256076 | ||||||||||||||||
| The only acceptable method of sending Validation Templates is through the QualityNet Secure Portal Secure File Transfer Mailbox. | ||||||||||||||||
| Validation Templates contain Protected Health Information (PHI) and cannot be sent via personal email -- even if a template were sent encrypted from a secure | ||||||||||||||||
| workplace email, it would still be considered a security violation. | ||||||||||||||||
| It is recommended to submit Validation Templates at least a week prior to the submission deadline in case there are difficulties with | ||||||||||||||||
| transmitting files and to allow time for revisions/corrections when necessary. | ||||||||||||||||
| If you are unable to log in to the Secure Portal, the first person to contact is your hospital's QualityNet Security Administrator. | ||||||||||||||||
| If your Security Administrator is unable to reestablish your access, you will need to contact the QualityNet HelpDesk at (866) 288-8912. | ||||||||||||||||
| It is recommended hospitals have two QualityNet Security Administrators at all times to ensure the ability to upload Validation | ||||||||||||||||
| Templates by the established submission deadlines. | ||||||||||||||||
| TEMPLATE COMPLETION & SUBMISSION TIPS | ||||||||||||||||
| Prior to submitting Validation Templates to CMS, it is recommended that quality assurance is performed on the data within the template. | ||||||||||||||||
| Review the [Definitions] tab to ensure correct information is entered in each field. | ||||||||||||||||
| ü | Do not add, delete, rename, or change the order of the tabs. | |||||||||||||||
| ü | Do not add, delete, or rename column headings. | |||||||||||||||
| ü | Do not leave the first row blank or skip rows between patient data. | |||||||||||||||
| ü | Make sure the State field contains the 2 character abbreviation for your state, not the full state name. | |||||||||||||||
| ü | Verify the Calendar Quarter listed on each Validation Template is correct. | |||||||||||||||
| ü | Review all dates for accuracy and correct format as specified on the [Definitions] tab. | |||||||||||||||
| ü | If a patient has not been discharged from the hospital, enter ‘Not Discharged’ for the Discharge Date field. | |||||||||||||||
| ü | Perform quality check of data entered into this template against what was entered into NHSN; stay mindful of differing CMS and NHSN deadlines. | |||||||||||||||
| ü | Check to ensure any cases with a separate Inpatient Rehabilitation Facility (IRF) or Inpatient Psychiatric Facility (IPF) CCN are not included on the template. | |||||||||||||||
| ü | Append the file name with the 6-digit CMS Certification Number (CCN)/Provider ID, followed by an underscore and the quarter. | |||||||||||||||
| For example: 012345_3QYY_CDI_ValidationTemplate.xlsx | ||||||||||||||||
| • When submitting templates via the [Compose Mail] button under the Mailbox section on the Secure File Transfer screen, input the subject of the message | ||||||||||||||||
| with the 6-digit CCN/Provider ID, Submission Quarter, and Template type(s) attached. | ||||||||||||||||
| For example: CCN 012345 3QYY MRSA & CDI Validation Templates | ||||||||||||||||
| • When choosing recipients, do NOT select any individual person(s) from the recipient list; only select the "VALIDATION CONTRACTOR" recipient. | ||||||||||||||||
| Individual accounts are not regularly monitored—sending to any one individual risks delay in processing. | ||||||||||||||||
| • As soon as the Validation Support Contractor has downloaded the template(s), Secure File Transfer will deliver an automatic email letting the submitter | ||||||||||||||||
| know the file has been downloaded. After a file has been downloaded, it will be in the queue for processing. | ||||||||||||||||
| • It is suggested that users verify a message has been sent by clicking on the [Sent] link under the Mailbox section of the Secure File Transfer screen. | ||||||||||||||||
| The message should be in your Sent folder with a status of "Received". | ||||||||||||||||
| NOTE: It typically takes 10 or more minutes for messages to appear in the Sent folder with a "Received" status. Please, do NOT re-send messages | ||||||||||||||||
| multiple times, as this significantly delays processing and requires version confirmation. | ||||||||||||||||
| • You will receive email confirmation (usually within 2 business days of being downloaded) from the Validation Support Contractor letting you know the Validation | ||||||||||||||||
| Templates were processed. If you do not receive a processing confirmation, please include your hospital's 6-digit CCN/Provider ID in an | ||||||||||||||||
| email to | Validation@hcqis.org. | |||||||||||||||
| File Type | application/vnd.openxmlformats-officedocument.spreadsheetml.sheet |
| File Modified | 0000-00-00 |
| File Created | 0000-00-00 |
© 2026 OMB.report | Privacy Policy